随着腹腔镜设备及技术水平的提高,急性期复杂的胆囊切除术已经不是腹腔镜手术的禁忌,但在胆囊三角解剖结构紊乱、与周围组织致密粘连的情况下,实施标准的腹腔镜下胆囊切除具有较大难度和风险,发生出血、胆管损伤及中转开腹的几率明显增加[1-4]。基于这种情况,许多学者提出采用腹腔镜下胆囊大部切除(laparoscopic subtotal cholecystectomy,LSC)的手术方式,即指仅将胆囊底部、体部及颈部前壁切除,保留靠近肝脏胆囊床和(或)紧贴胆囊三角的部分后壁,闭合胆囊颈管的手术方式[5-8]。前期许多文献[9-11]报道显示,该术式可降低手术难度,减少中转开腹手术率,并可有效避免胆管、血管损伤。但是这种手术方式面临的主要问题是胆囊颈管情况不明及结石残留,导致术后需要二期治疗干预的情况增加[12-13]。为解决这一问题,笔者单位在采用LSC进行复杂胆囊切除手术的同时,应用胆道镜探查胆道颈管并处理结石,取得了较好的效果。本研究通过回顾性分析LSC中应用胆道镜患者的临床资料,评价胆道镜探查胆囊颈管的安全性和有效性,并介绍LSC中处理胆囊颈管结石的方法,以期为临床实施复杂的胆囊切除提供决策参考。
1 资料与方法
1.1 一般资料
2014年1月—2018年1月,大连大学附属中山医院胆石病微创外科为36例胆囊三角粘连严重的患者实施LSC,同时采用胆道镜对胆囊颈管进行探查。本组男11例,女25例;年龄22~72岁,平均年龄56.3岁;急性化脓性胆囊炎22例,急性坏疽性胆囊炎5例,慢性萎缩性胆囊炎9例。术前所有患者均行超声及CT检查明确诊断,33例患者进行MRCP检查,其中28例提示胆囊颈管内结石或可疑结石,2例患者合并Mirriz综合征。
1.2 胆道镜探查胆囊管指征
⑴ 术前影像学资料提示胆囊管内结石或可疑结石,术中胆囊管开口处未见结石;⑵ 胆囊管开口处无胆汁流出;⑶ 腹腔镜下观察胆囊管内存在结石,常规腹腔镜器械无法取出结石;⑷ 常规腹腔镜器械取出结石,胆道管内仍无胆汁流出。
1.3 手术方法
仰卧位,给予气管插管静吸复合全身麻醉,建立气腹,在脐旁做切口,作穿刺孔10 mm,建立气腹压12 mmHg(1 mmHg=0.133 kPa),气腹建立后将30°置入腹腔镜,在腹腔镜监视下作另外2个穿刺孔,对于肥胖、胆囊三角处显露困难患者,在右腋前线增加穿刺孔,放置Trocar和相关器械。术中观察胆囊壁显著增厚,胆囊三角粘连紧密,无法进行分离,分离胆囊与粘连的大网膜及肠管,显露胆囊底体至胆囊壶腹部,穿刺抽出胆囊内脓性胆汁或白胆汁,自胆囊体靠近壶腹部剖开,取出胆囊内结石,胆道镜在胆囊腔内观察胆囊颈管开口位置,利用自制圆锥型胆道镜吸附器引导胆道镜进入胆囊颈管观察(图1),发现结石采用取石网篮取出,如遇胆囊颈管结石嵌顿难以取出,可置入等离子碎石器进行碎石后取出,如结石被胆囊管螺旋瓣包裹紧密,无法有效碎石,可在胆道镜下采用针刀适度剖开胆囊颈管内螺旋瓣,显露结石后进行碎石、取石(图2-4),取净结石可见金黄色胆汁自胆囊管涌出,尽可能深度探查胆囊颈管,退出胆道镜,保留胆囊三角处胆囊壁,切除胆囊底体、壶腹部胆囊,将残留后壁胆囊黏膜进行电刀烧灼,采用4-0可吸收倒刺线连续缝扎胆囊颈管开口处,于肝下胆囊颈管缝合附近放置引流管。
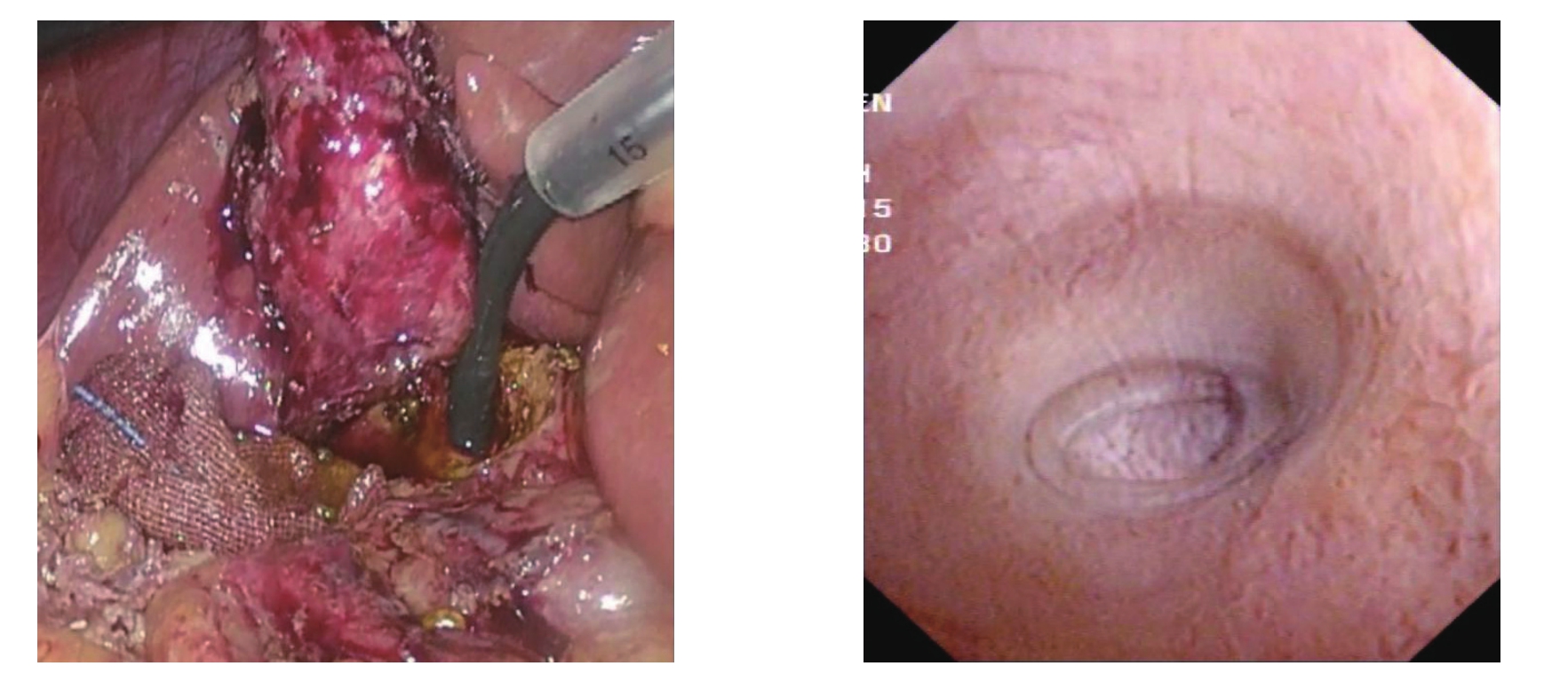
图1 胆道镜插入胆囊颈管内观察胆囊颈管内部情况
Figure 1 Insertion of the choledochoscope into the neck of the gallbladder to observe the internal condition of the neck of the gallbladder
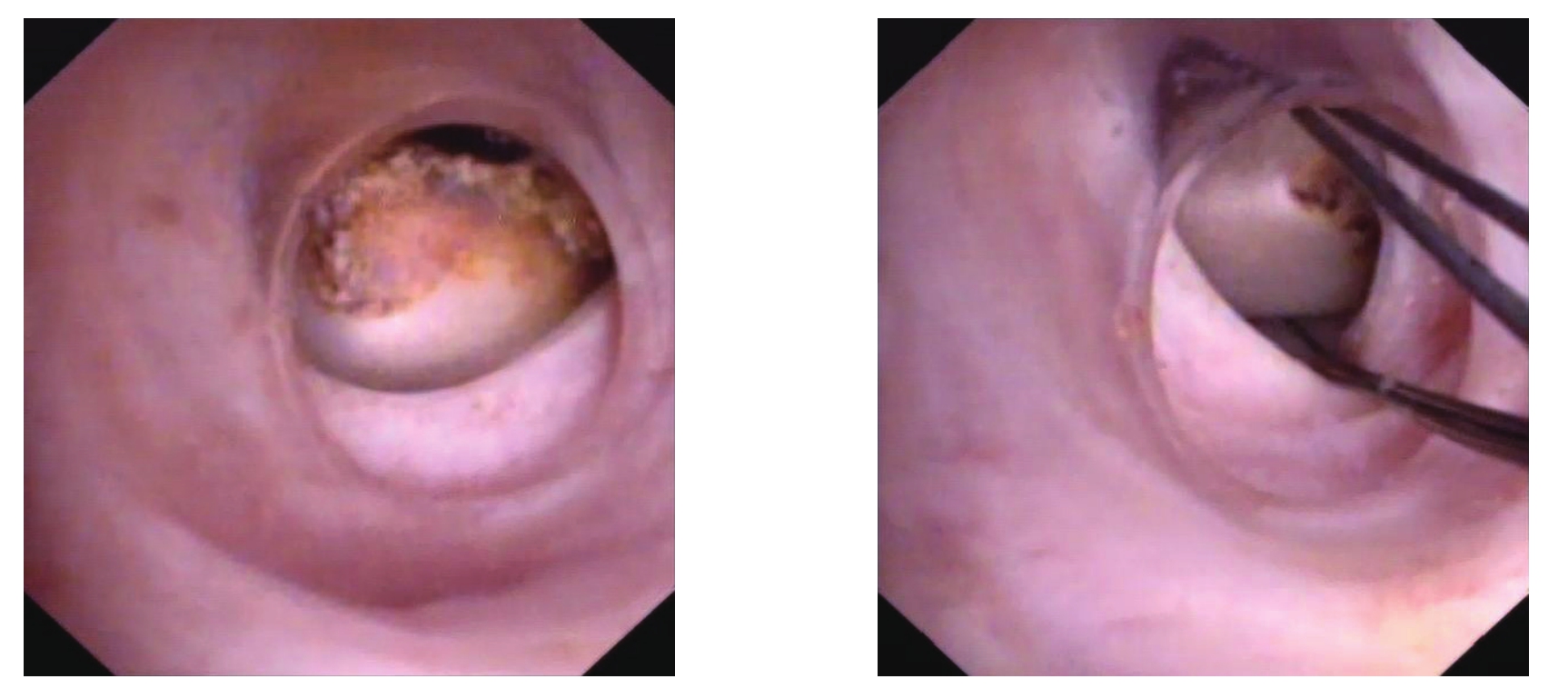
图2 胆道镜发现胆囊管内结石,采用取石网篮取石
Figure 2 Stones found by choledochoscopy in the cystic duct and extracted with a stone basket

图3 胆囊管内嵌顿结石,采用等离子碎石取石后,胆汁自胆囊管内涌出
Figure 3 Stone incarceration in the cystic duct, and bile outflow from the cystic duct after plasma lithotripsy
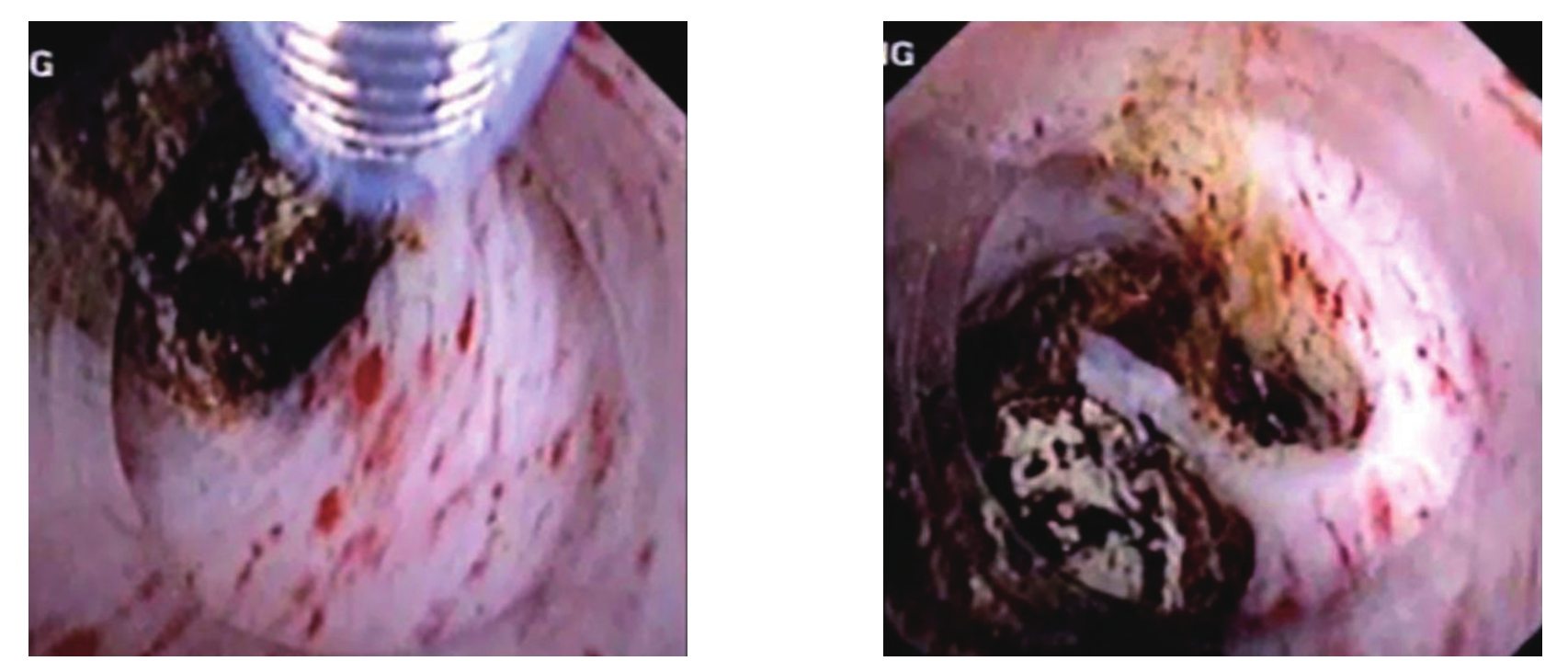
图4 胆囊管嵌顿结石,采用针刀剖开螺旋瓣后取石
Figure 4 Incarcerated stone in the cystic duct and stone removal after Heister spiral valve incision with a needle knife
2 结 果
2.1 患者术中情况
本组实施LS C同时进行胆囊管胆道镜探查36例,术中发现胆囊颈管内有胆汁流出8例,无胆汁流出28例;有胆汁流出患者经过胆囊颈管探查发现结石2例,采用超细取石网篮取出;无胆汁流出患者胆道镜探查发现结石26例,观察到胆囊管远端炎性狭窄1例,胆囊管迂曲无法进一步深入探查1例;针对胆囊管内结石:单纯采用取石网篮取出4例,采用等离子碎石+取石网篮取石16例,采用针刀剖开胆囊管螺旋瓣+等离子碎石+取石6例;取石后胆汁流出23例,3例无胆汁流出,其中1例远端炎性狭窄,考虑胆囊管炎性闭塞,另2例胆管扭曲,未能完成进一步探查明确原因。35例胆囊颈管采用倒刺线进行关闭,1例因胆囊颈管炎症水肿严重,无法缝合,颈管内放置引流管。无中转开腹者,术中无胆管及血管损伤发生。手术时间50~170 min,术中出血量50~120 mL。
2.2 患者术后情况
7例患者出现并发症,其中包括胆总管结石胆管炎1例,胆汁漏2例,Trocar孔感染1例,其他非手术相关并发症4例;行ERCP胆总管取石1例,胆汁漏患者保持引流管通畅,分别于2周和1个月后胆汁漏停止。所有患者术后出院时间为5~10 d。随访5个月至1年,无手术相关并发症出现。
3 讨 论
腹腔镜胆囊切除是治疗胆囊结石伴胆囊炎的金标准手术,但当胆囊三角严重炎症水肿、粘连或者纤维化、甚至形成致密疤痕组织时,对肝总管、胆总管、胆囊管等“三管”及胆囊床解剖结构的辨别和分离存在较大的困难,若强行切除胆囊,容易损伤胆管、肝脏。2018年东京急性胆囊炎治疗指南建议选择合适的替代手术方案[14-15],包括中转开放手术、LSC。许多学者倾向认为LSC优于开腹手术[9-11],其理由是中转开腹手术相对于腹腔镜手术,并不能很好提供胆囊三角部位解剖观察和分离,多数患者仍然需要实施胆囊大部切除术[14,16],并且目前许多医生并没有足够开腹胆囊切除的手术经验。而LSC其近期术后患者恢复时间及患者舒适度明显高于开腹手术[17-18],而其远期的治疗效果,较LC手术相类似[19]。
LSC实施过程中胆囊颈管的处理是该术式的一个难点,多数学者在腹腔镜直视下判断胆囊颈管情况,若发现胆囊颈部结石嵌顿,可于Hartmann袋处切开取石;如因嵌顿结石导致解剖结构不清,可向上在胆囊体部横行切开取石,从胆囊内部观察胆囊颈管开口位置[20-22]。若胆囊管开口处持续10 min无胆汁流出,终止手术,放置腹腔引流;若胆囊管开口处有胆汁流出,可在开口处插入硬膜外麻醉导管或9-F细引流管,深入胆囊管,行术中胆道造影了解下端胆囊管通畅情况[23-25];也有学者[26]建议术中应用胆道探条判断胆囊颈管有无结石残留;或者向胆囊管注入适量生理盐水,明确胆囊管是否通畅[27]。 但上述操作方法弊病是无法清晰了解胆囊颈管的情况,在无胆汁流出的情况,无法准确判断胆囊颈管是炎性自截还是有结石嵌顿;在胆囊颈管与胆总管关系不清楚的情况下,贸然向下延长胆囊颈管切口,有损伤十二指肠或胆总管风险。并且如果嵌顿结石深在,常规方法很难将结石取出、取净,这些情况也导致该术式胆囊颈管残留结石率为3.1%[28],明显高于标准胆囊切除术的0.3%,有研究[29-30]也显示,该手术方式术后需要内镜干预、穿刺引流及外科再手术的情况也高于标准胆囊切除患者。因此对于胆囊颈管的探查具有非常重要意义。术中胆囊管造影对于了解胆囊颈管情况有一定意义,但对于胆囊颈管结石与炎症狭窄鉴别能力有限,并且即便发现胆囊管内存在结石,在处理上仍存在很大困难。
在本组36例实施LSC患者中,笔者尝试采用胆道镜或超细胆道镜对胆囊颈管进行探查,胆道镜经过胆囊腔内进入胆囊管,可以准确了解胆囊管开口位置及大致走行,不对胆囊三角进行分离,从而有效避免了胆总管、副肝管、十二指肠等器官的损伤。胆道镜进入胆囊管可以直接观察到胆囊管内情况,利用胆道镜下的取石、碎石设备和技术可更好处理胆囊颈管嵌顿结石,通过胆囊管探查结果发现,胆囊管内有胆汁流出,并不能保证胆囊管无结石残留,本组8例胆囊管有胆汁流出患者,因术前MRCP提示胆囊管内可疑结石,对胆囊管采用胆道镜检查,发现2例患者存在结石;而无胆汁流出的胆囊颈管内多有结石嵌顿,而非炎症自截情况。本组28例术中无胆汁流出的胆囊管,经胆道镜探查发现26例明确为结石嵌顿,仅有1例观察到胆囊颈管远端炎性闭塞改变。经过取石操作后多可见金黄色胆汁流出。此外,胆囊管的正确处理是该手术的重要步骤,通过对胆囊颈管的胆道镜探查,可以较好了解胆囊颈管走行及与周围组织关系,为接下来缝扎胆囊颈管提供安全的进针深度及缝合范围。
腹腔镜下采用胆道镜探查胆囊颈管在操作上具有一定难度,需要具有良好的腹腔镜下胆道镜的操作技术和一定的经验积累,胆道镜在腹腔内缺乏力臂支撑,进入胆囊颈管有一定难度,笔者在实践中采用34号胸科引流管作为支撑,伸入到胆囊颈管开口处,也可采用胆道镜把持钳辅助进入胆道镜;胆囊颈管腔狭小、存在多个螺旋瓣、走行迂曲,常规胆道镜很难进入,为此采用圆锥形透明帽戴在胆道镜头端,透明帽尖端可以很好进入胆囊管腔,通过旋转胆道镜可以逐个通过螺旋瓣,实现对胆囊颈管最大程度探查;对于嵌顿结石,取石网篮无法弹开,造成取石失败,此时可采用高频针刀,抵住嵌顿结石表面的螺旋瓣进行剖开,达到结石松动,如结石较大,可进行等离子碎石,此时尽量减少胆道镜注水,避免结石碎屑进入胆总管,取净结石后多数情况可见金黄色胆汁涌出,表明胆囊颈管通畅。
在采用胆道镜探查胆囊颈管的操作实践中,笔者也认识到,由于胆囊颈管狭窄及迂曲,该方法只能最大限度探查胆囊颈管,不能保证胆囊颈管全程探查及结石取净,本组有2例患者未能明确无胆汁流出原因,其中有1例患者术后出现寒战、发热,化验胆红素升高,MRCP提示胆总管结石,考虑可能是胆囊管内结石移位所致,该患者行ERCP治疗获得治愈;此外,术中使用胆道镜,增加了胆汁进入腹腔的几率,应及时吸出腹腔内胆汁,同时要放置腹腔引流管,防止隔下感染及迟发性胆汁漏的发生。
综上所述,采用LSC结合胆道镜探查胆囊颈管,可以最大程度了解胆囊颈管内情况,较好解决胆囊颈管结石嵌顿的情况、最大程度避免胆囊颈管遗漏结石,在复杂胆囊手术中具有一定应用价值。同时也认识到,胆道镜辅助LSC多数情况并非必须,只有在胆囊体、壶腹部显著粘连、胆囊管结石嵌顿难以取出等特殊情况下才考虑应用。
[1] 施凉潘, 黄顺涵, 郑志华, 等.急性重症胆囊炎手术时机选择分析[J].中国普通外科杂志, 2018, 27(2):225-230.doi:10.3978/j.issn.1005-6947.2018.02.015.Shi LP, Huang SH, Zheng ZH, et al.Analysis of surgical timing for acute severe cholecystitis[J].Chinese Journal of General Surgery,2018, 27(2):225-230.doi:10.3978/j.issn.1005-6947.2018.02.015.
[2] 孙明明, 范逸怡, 党胜春.早期不同时间点行腹腔镜胆囊切除术治疗急性结石性胆囊炎疗效及安全性的Meta分析[J].中国普通外科杂志, 2017, 26(8):1019-1029.doi:10.3978/j.issn.1005-6947.2017.08.010.Sun MM, Fan YY, Dang SC.Efficacy and safety of laparoscopic cholecystectomy in treatment of acute calculous cholecystitis at different timing within early stage: a Meta-analysis[J].Chinese Journal of General Surgery, 2017, 26(8):1019-1029.doi:10.3978/j.issn.1005-6947.2017.08.010.
[3] 史洪石, 靳君华, 赵海平.经皮经肝胆囊穿刺引流术在胆囊炎急性发作治疗中的应用现状[J].中国普通外科杂志, 2018,27(2):236-240.doi:10.3978/j.issn.1005-6947.2018.02.017.Shi HS, Jin JH, Zhao HP.Current status of application of percutaneous transhepatic gallbladder puncture and drainage in treatment of cholecystitis in acute stage[J].Chinese Journal of General Surgery, 2018, 27(2):236-240.doi:10.3978/j.issn.1005-6947.2018.02.017.
[4] 谢伟选, 罗昆仑.胆囊切除术联合腹腔镜下胆总管探查术后胆总管一期缝合与T管引流的疗效比较[J].中国普通外科杂志, 2019,28(2):127-134.doi:10.7659/j.issn.1005-6947.2019.02.001.Xie WX, Luo KL.Efficacy comparison between primary closure and T-tube drainage following laparoscopic cholecystectomy with common bile duct exploration[J].Chinese Journal of General Surgery, 2019, 28(2):127-134.doi:10.7659/j.issn.1005-6947.2019.02.001.
[5] 时吉庆, 侯玲, 李俊, 等.腹腔镜胆囊大部切除术临床应用体会[J].肝胆胰外科杂志, 2016, 28(4):322-323.doi:10.11952/j.issn.1007-1954.2016.04.016.Shi JQ, Hou L, Li J, et al.Clinical experience in laparoscopic subtotal cholecystectomy[J].Journal of Hepatopancreatobiliary Surgery, 2016, 28(4):322-323.doi:10.11952/j.issn.1007-1954.2016.04.016.
[6] 徐素琴, 邹书兵.腹腔镜胆囊切除术相关胆管损伤的研究进展[J].中国普通外科杂志, 2019, 28(2):227-233.doi:10.7659/j.issn.1005-6947.2019.02.014.Xu SQ, Zou SB.Research progress of bile duct injury associated with laparoscopic cholecystectomy[J].Chinese Journal of General Surgery, 2019, 28(2):227-233.doi:10.7659/j.issn.1005-6947.2019.02.014.
[7] 姚宇驰, 商中华.腹腔镜胆囊切除术联合腹腔镜胆总管探查术中转开腹的危险因素探讨及临床分析[J].中国普通外科杂志,2018, 27(8):989-997.doi:10.3978/j.issn.1005-6947.2018.08.007.Yao YC, Shang ZH.Risk factors for open conversion in patients undergoing laparoscopic cholecystectomy combined with common bile duct exploration and relevant clinical analysis[J].Chinese Journal of General Surgery, 2018, 27(8):989-997.doi:10.3978/j.issn.1005-6947.2018.08.007.
[8] 周晓春.腹腔镜下胆囊大部分切除术临床研究[J].中国临床医生, 2014, 42(12):71-72.doi:10.3969/j.issn.1008-1089.2014.12.031.Zhou XC.Clinical analysis of laparoscopic subtotal cholecystectomy[J].Chinese Journal for Clinicians, 2014,42(12):71-72.doi:10.3969/j.issn.1008-1089.2014.12.031.
[9] 孙文兵.重度急性胆囊炎急诊腹腔镜手术时胆管损伤的预防策略[J].中华肝胆外科杂志, 2016, 22(7):433-436.doi:10.3760/cma.j.issn.1007-8118.2016.07.001.Sun WB.Prevention strategy of bile duct injury in emergency laparoscopic surgery for severe acute cholecystitis[J].Chinese Journal of Hepatobiliary Surgery, 2016, 22(7):433-436.doi:10.3760/cma.j.issn.1007-8118.2016.07.001.
[10] Tian Y, Wu SD, Su Y, et al.Laparoscopic subtotal cholecystectomy as an alternative procedure designed to prevent bile duct injury:Experience of a hospital in northern China[J].Surg Today, 2009,39(6):510-513.doi:10.1007/s00595-008-3916-2.
[11] Singhal T, Balakrishnan S, Hussain A, et al.Laparoscopic subtotal cholecystectomy: Initial experience with laparoscopic management of difficult cholecystitis[J].Surgeon, 2009, 7(5):263-268.doi:10.1016/s1479-666x(09)80002-4.
[12] Lidsky ME, Speicher PJ, Ezekian B, et al.Subtotal cholecystectomy for the hostile gallbladder: failure to control the cystic duct results in significant morbidity[J].HPB, 2017, 19(6):547-556..doi:10.1016/j.hpb.2017.02.441.
[13] 江伟廷, 杨志英, 寇玉彬.一组腹腔镜胆囊大部切除术病例的术后随访观察[J].中华腔镜外科杂志:电子版, 2014, 7(5):402-403.doi:10.3877/cma.j.issn.1674-6899.2014.05.016.Jiang WT, Yang ZJ, Kou YB.Value of laparoscopic subtotal resection in laparoscopic cholecystectomy[J].Chinese Journal of Laparoscopic Surgery: Electronic Edition, 2014, 7(5):402-403.doi:10.3877/cma.j.issn.1674-6899.2014.05.016.
[14] 张宇华.急性胆道感染《东京指南(2018)》拔萃[J].中国实用外科杂志, 2018, 38(7):767-774.doi:10.19538/j.cjps.issn 1005-2208 2018.07.16.Zhang YH.Interpretation of Tokyo Guidelines 2018 for management of acute cholangitis and cholecystitis[J].Chinese Journal of Practical Surgery, 2018, 38(7):767-774.doi:10.19538/j.cjps.issn 1005-2208 2018.07.16.
[15] 董汉华, 武齐齐, 陈孝平.急性胆道感染东京指南(2018版)更新解读[J].临床外科杂志, 2019, 27(1):5-9.doi:10.3969/j.issn.1005-6483.2019.01.001.Dong HH, Wu QQ, Chen XP.Interpretation of Tokyo Guidelines(2018) for management of acute infection of biliary tract[J].Journal of Clinical Surgery, 2019, 27(1):5-9.doi:10.3969/j.issn.1005-6483.2019.01.001.
[16] Diamond T, Mole DJ.Anatomical orientation and cross-checking—the key to safer laparoscopic cholecystectomy[J].Br J Surg, 2005,92(6):663-664.doi:10.1002/bjs.4992.
[17] Hubert C, Annet L, Van Beers BE, et al.The “inside approach of the gallbladder” is an alternative to the classic Calo's triangle dissection for a safe operation in severe cholecystitis[J].Surg Endosc, 2010, 24(10):2626-2632.doi: 10.1007/s00464-010-0966-5.
[18] Henneman D, da Costa DW, Vrouenraets BC, et al.Laparoscopic partial cholecystectomy for the difficult gallbladder: a systematic review[J].Surg Endosc, 2013, 27(2):351-358.doi:10.1007/s00464-012-2458-2.
[19] Supit C, Supit T, Mazni Y, et al.The outcome of laparoscopic subtotal cholecystectomy in difficult cases - A case series[J].Int J Surg Case Rep, 2017, 41:311-314.doi: 10.1016/j.ijscr.2017.10.054.
[20] 邬叶锋, 赵登秋.胆囊嵌顿性结石行腹腔镜胆囊切除术138例体会[J].肝胆胰外科杂志, 2018, 30(3):245-247.doi:10.11952/j.issn.1007-1954.2018.03.016.Wu YF, Zhao DQ.Laparoscopic cholecystectomy for incarcerated stones in gallbladder: experience in 138 cases[J].Journal of Hepatopancreatobiliary Surgery, 2018, 30(3):245-247.doi:10.11952/j.issn.1007-1954.2018.03.016.
[21] 张长和, 田野, 曹晓飞, 等.经胆囊颈横断腹腔镜胆囊次全切除在复杂性胆囊切除术中应用32例体会[J].中国实用外科杂志, 2017,37(9):1045-1046.doi:10.19538/j.cjps.issn1005-2208.2017.09.26.Zhang CH, Tian Y, Cao XF, et al.Application of laparoscopic subtotal cholecystectomy by transverse through the neck of the gallbladder in complex cholecystectomy: experience in 32 cases[J].Chinese Journal of Practical Surgery, 2017, 37(9):1045-1046.doi:10.19538/j.cjps.issn1005-2208.2017.09.26.
[22] 陈宏亮, 彭成初, 彭永海.腹腔镜胆囊大部切除术的技术要点探讨[J].腹腔镜外科杂志, 2010, 15(4):311-312.Chen HL, Peng CC, Peng YH.Technique of laparoscopic subtotal cholecystectomy[J].Journal of Laparoscopic Surgery, 2010,15(4):311-312.
[23] 陈仪, 刘习红.腹腔镜胆囊大部切除术的临床分析[J].中国医药指南, 2011, 9(15):222-223.doi:10.3969/j.issn.1671-8194.2011.15.172.Chen Y, Liu XH.Clinical analysis of laparoscopic subtotal cholecystectomy[J].Guide of China Medicine, 2011, 9(15):222-223.doi:10.3969/j.issn.1671-8194.2011.15.172.
[24] 秦建伟, 高静涛, 龚振斌, 等.腹腔镜胆囊大部切除术中胆囊管残端的处理[J].腹腔镜外科杂志, 2010, 15(12):902-903.doi:10.3969/j.issn.1009-6612.2010.12.008.Qin JW, Gao JT, Gong ZB, et al.Management of cholecystic duct remnant in laparoscopic subtotal cholecystectomy[J].Journal of Laparoscopic Surgery, 2010, 15(12):902-903.doi:10.3969/j.issn.1009-6612.2010.12.008.
[25] 任玉征, 胡伟, 黄永斌.开放性胆囊大部切除术治疗慢性胆囊炎临床疗效观察[J].中国现代医生, 2013, 51(6):112-113.Ren YZ, Hu W, Huang YB.Clinical observation on the treatment of chronic cholecystitis of open subtotal cholecystectomy surgery[J].China Modern Doctor, 2013, 51(6):112-113.
[26] 邓治国, 张勇, 吴赛红.腹腔镜胆囊大部分切除术术中处理冰冻样胆囊床及胆囊三角的手术技巧和体会[J].中外医疗, 2011,30(33):15-16.doi:10.3969/j.issn.1674-0742.2011.33.008.Deng ZG, Zhang Y, Wu SH.Laparoscopic resection of the gallbladder most treatment during operation frozen samples and gallbladder triangle gallbladder bed surgical skills and experience[J].China Foreign Medical Treatment, 2011, 30(33):15-16.doi:10.3969/j.issn.1674-0742.2011.33.008.
[27] 郭欣, 吕小慧, 陈芦斌.腹腔镜胆囊大部切除术的临床应用体会(附468例报告)[J].中国内镜杂志, 2017, 23(10):95-97.doi:10.3969/j.issn.1007-1989.2017.10.020.Guo X, Lu XH, Chen LB.Clinical experience of laparoscopic subtotal cholecystectomy (468 cases)[J].China Journal of Endoscopy, 2017, 23(10):95-97.doi:10.3969/j.issn.1007-1989.2017.10.020.
[28] Elshaer M, Gravante G, Thomas K, et al.Subtotal Cholecystectomy for "Difficult Gallbladders" Systematic Review and Metaanalysis[J].JAMA Surg, 2015, 150(2):159-168.doi:10.1001/jamasurg.2014.1219.
[29] 江培朝, 李玉华, 姬涛, 等.经皮肝胆囊穿刺引流术联合腹腔镜胆囊切除手术治疗急性重症胆囊炎的临床疗效分析[J].中华医院感染学杂志, 2017, 27(11):2528-2531.doi:10.11816/cn.ni.2017-170101.Jiang PC, Li YH, Ji T, et al.Clinical efficacy of PTGBD combined with LC in the treatment of acute critical cholecystitis[J].Chinese Journal of Nosocomiology, 2017, 27(11):2528-2531.doi:10.11816/cn.ni.2017-170101.
[30] 赵红光, 刘凯, 刘亚辉.经皮经肝胆囊穿刺引流术后择期行腹腔镜胆囊切除术治疗60岁以上急性重症胆囊炎患者的最佳时机探讨[J].临床肝胆病杂志, 2017, 33(4):705-710.doi:10.3969/j.issn.1001-5256.2017.04.021.Zhao HG, Liu K, Liu YH.The most appropriate timing for selective laparoscopic cholecystectomy after percutaneous transhepatic gallbladder drainage in patients with acute severe cholecystitis aged above 60 years[J].Journal of Clinical Hepatology, 2017, 33(4):705-710.doi:10.3969/j.issn.1001-5256.2017.04.021.
