肝胆管结石因其高残余率、高复发率等,一直是肝胆外科手术中的难点[1-2]。复杂肝胆管结石患者往往行多次手术治疗,然而随着多次手术以及反复发作胆管炎,许多肝内胆管结石患者合并二级以上胆管的狭窄以及不同程度肝萎缩肥大综合征[3-4]。传统手术以切除肝脏来解决二级以上胆管狭窄的问题,但反复结石复发、多次手术等所致肝硬化、肝比例失调,使剩余肝体积不足[5]。我院继提出“切除病肝、取尽结石、解除狭窄、矫治畸形、通畅引流”的20字原则后提出“保肝保胆”理念,针对高位胆管狭窄采用肝方叶切除联合肝门胆管高位劈开整形、胆肠内引流手术治疗36例不同程度的肝门部胆管狭窄患者,尽可能的保留了正常肝组织,手术效果良好,现报告如下。
1 资料与方法
1.1 一般资料
回顾性分析湖南省人民医院肝胆外科2015年7月—2019年6月36例行肝方叶切除、肝门胆管高位劈开整形、胆肠内引流手术的肝门胆管狭窄合并结石患者的临床资料。其中男15例,女21例;平均年龄52.5岁。36例患者均有不同程度的上腹部疼痛病史,21例出现发热,14例就诊时已有黄疸。既往平均手术2.4次,既往手术原因包括肝胆管结石29例,其中行胆囊切除、胆道探查16例,肝脏部分切除者10例,胆肠内引流者7例,平均复发时间为4年。医源性胆道损伤2例,均为胆囊手术胆道损伤,术后5年余再生结石。5例胆总管囊肿行胆肠内引流术。36例患者均存在不同程度肝方叶肥大、肝门部胆管狭窄,其中 肝门胆管汇合部狭窄18例,合并右肝管狭窄8例,合并左肝管狭窄10例。术前肝功能分级Child A级28例,Child B级8例;5例因急性梗阻性化脓性胆管炎术前放置鼻胆管引流,3例行PTCD引流减黄。以手术方式为入组标准, 均行开腹肝方叶切除联合肝门胆管高位劈开整形、胆肠内引流手术。
1.2 术前评估
术前常规行腹部B超、CT、磁共振等检查(图1),评估肝功能、肝硬化程度、肝脏形态及肝体积、营养状况等情况,明确胆管狭窄位置;对于明显黄疸或者合并急性胆管炎的患者实施PTCD术或者鼻胆管引流术;手术治疗遵循原20字原则+“保肝保胆”的24字原则。

图1 术前CT检查资料 A:CT平扫见干比例严重失调,胆管扩张合并积气、结石;B:增强扫描示第一肝门处血管曲张明显
Figure 1 Preoperative CT scan images A: CT plain scan showing severe imbalance of dry ratio, and biliary dilatation with gas and stones;B: Enhanced CT scan showing obvious varicose veins at the first hilum
1.3 手术适应证
⑴ 肝方叶肥大,遮挡肝门胆管;⑵ 二级以上胆管狭窄合并肝内胆管结石,且肝脏无萎缩纤维化;⑶ 肝体积缩小,不宜行大范围切肝者;⑷ 肝比例失调、肝门旋转者。
1.4 手术步骤
常规取右上腹“J”型切口或原手术切口, 探查腹腔内主要脏器,显露第一肝门、预置Pringle阻断带,细针穿刺抽到胆汁明确胆总管或肝门胆管位置后,“四边法”(边缝合边切开)打开胆管,取尽胆总管内结石,向上劈开肝总管,探查肝门部胆管有无狭窄,若发现有明显狭窄,预计会要行胆肠内引流,则予以横断胆总管,向下剥离胆总管至胰腺上缘水平,离断胆总管后(离断前需要确认胆总管下段通畅且无结石残留),Prolene线连续缝合关闭远端胆总管;再降低肝门板,沿肝圆韧带途径进一步显露左肝管和切断肝桥。如果肝方叶阻碍肝门胆管的显露和高位劈开,予以切除肥大的肝方叶(图2A),以充分显露肝门部胆管,此时右肝胆管的开口往往也可以得到更好的显露,但必要时仍可以沿胆囊床途径或者Rouviere沟(右肝后叶胆管)途径等向右高位劈开右侧的胆管口,以彻底的敞开肝门部狭窄(图2B-C)。
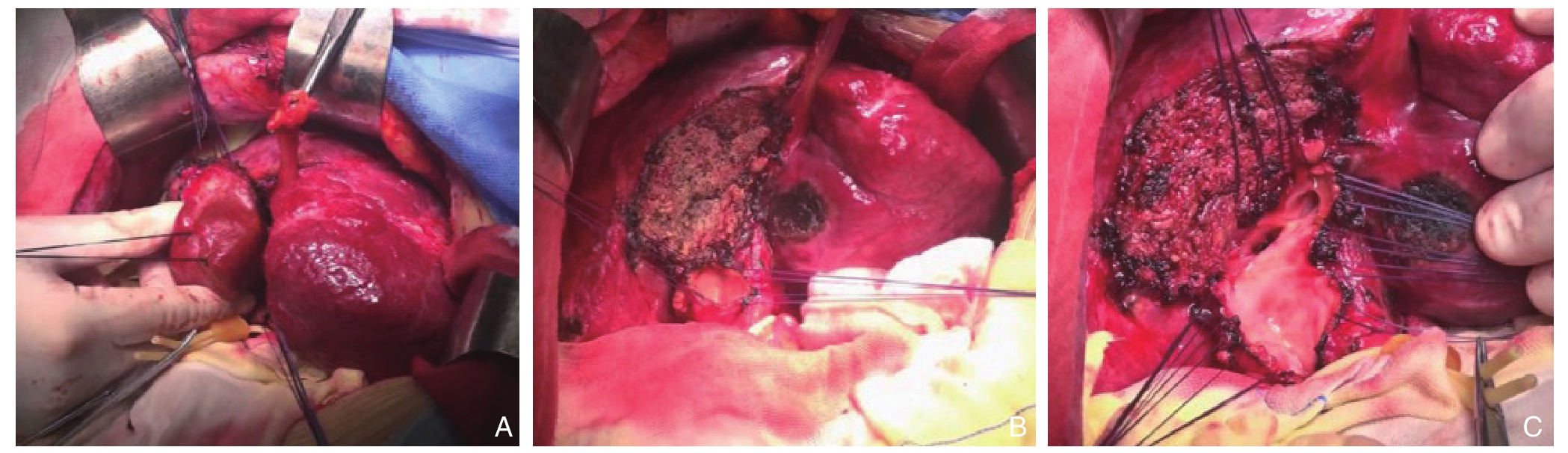
图2 术中图片 A:肥大的肝方叶遮挡肝门;B:切除肝方叶后找到胆总管,利于显露肝门胆管;C:“四边法”(边缝合边切开)显露左右肝管
Figure 2 Intraoperative views A: Hypertrophic quadrate lobe of the liver covering the porta hepatis; B: Discovery of the common bile duct after resection of the hepatic quadrate lobe, and making for the exposure of the hilar bile ducts; C:Exposure of the left and right hepatic ducts by “four-sided method” (simultaneous suturing after incision)
探查肝内胆管情况并取石 ,如肝脏萎缩纤维化则予以切除,如肝脏质地良好,肝内更高位置的胆管狭窄(图3A),则可顺胆管方向切开有狭窄的胆管壁行“胆管内吻合”,其要点是沿肝内狭窄胆管的长轴方向,采取边缝合边切开的方式,逐步缝合并切开狭窄处的胆管壁,缝合的方向与切开的方向是相同的(图3B-C),以防止损伤伴行的门静脉分支和肝动脉分支,以期进一步解除肝内狭窄的胆管口。必要时使用胆道镜或者输尿管硬镜等探查肝内,必要时还可钬激光碎石,尽量取尽结石。拼合整形肝门部胆管,以形成一个完整的较大的肝胆管盆,后续行Roux-en-Y胆肠内引流[6]。
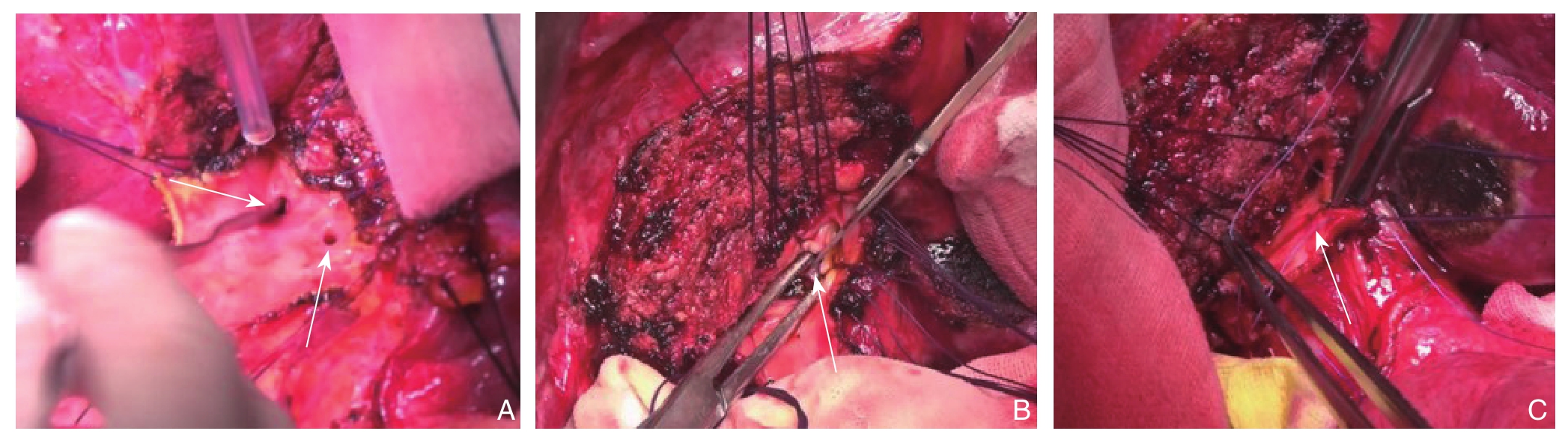
图3 术中“内吻合”图片 A:肝内更高位置的胆管狭窄;B:“四边法”顺胆管方向切开有狭窄的胆管壁;C:拼合相邻胆管,缝合的方向与切开的方向是相同的
Figure 3 Intraoperative internal anastomosis A: A higher stenosis of the intrahepatic bile duct; B: Incision of the wall of the stenostic bile duct in the direction of the bile duct by the "four-sided method"; C: Joining together the adjacent bile ducts in the same direction as the incision
2 结 果
2.1 患者手术情况
本组36例患者均行了肝方叶切除、肝门胆管高位劈开整形、胆肠内引流手术,术中采用取石钳取石、塑形管反复冲洗、胆道镜探查等多种方式取尽结石,平均手术时间354.4 min,平均失血量230.5 mL。术后平均结石清除率在90%以上(图4),术后由于残余结石再行胆道镜取石的患者有6例,此6例中有4例仅行1次胆道镜取石即拔除T管,有2例行2次胆道镜取石后拔除T管。
2.2 患者术后情况
术后平均住院天数为10.4 d,术后2例患者出现胆汁漏,经积极引流治疗后好转,3例患者出现切口脂肪液化、感染,1例患者不完全性肠梗阻,均保守治疗后好转,无围术期肝功能衰竭、死亡病例。术后采用门诊、电话随访12~48个月,4例患者出现反流性胆管炎,经保守治疗均可缓解,无胆肠吻合口再发狭窄病例。

图4 术后CT复查结果显示结石取尽
Figure 4 Postoperative CT scan showing complete removal of stones
3 讨 论
近年来,肝胆管结石的发病率呈逐渐下降趋势,但结石复发率达30%~60%[7-8]。结石复发与结石残留、手术方式不当、反复的胆管炎发作等相关[9-10]。复杂肝胆管结石常见于多次手术、结石复发、胆管炎反复发作的患者,再次手术的根本在于解除胆道狭窄,对于肝胆管结石多次手术后复发,如何最大限度的解除肝门甚至是肝内胆管狭窄,一直是胆道外科的难点和热点[1,11]。
复杂肝胆管结石多合并有胆汁性肝硬化、门静脉高压症、肝形态比例失调、胆瘘甚至是胆管癌等,经过不断的探索,目前手术治疗肝胆管结石的入肝途径主要有胆总管途径、胆囊床途径、肝圆韧带途径、左肝外叶途径等[12-13]。但多次手术后患者再次手术面临层次不清、肝门部静脉曲张、狭窄位置深、肝门部旋位等复杂问题,手术难度大,经以上经典的入肝途径虽可到达肝门,针对肝门处及以上胆管狭窄的病例,往往因肝方叶遮挡无法继续向上延伸、解除狭窄。本组36例患者因肝门部以上胆管狭窄或因肝内大量结石无法取尽,行肝方叶切除后联合肝圆韧带途径向左、右分别敞开胆管,解除狭窄后,形成肝胆管盆,利于取石和充分引流。
肝内胆管结石手术清除率在64.8%~90.9%不等,联合术后胆道镜等可提高结石清除率[14-15]。在我院肝胆医学中心在肝胆管结石的治疗过程中积累了一定的经验。本组36例患者均采用“四边法”打开胆总管后向上劈开胆管至肝门隆突后仍无法充分敞开狭窄的胆管,肥大的肝方叶阻碍进一步操作和取石,遂将该部分肝方叶切除后再充分敞开左、右肝内胆管。该方法切除的肝脏较小,能有效解除肝内胆管的狭窄,结石清除率在90%。与以往半肝切除、解剖性肝叶切除相比[16-17],同样可以最大限度的取尽结石,同时能很好的保存患者的有效肝脏[14,18],符合“保肝保胆”的治疗理念[19],进而避免术后肝功能衰竭。
行肝方叶切除后,对于肝内位置较深的胆管狭窄,完全切开狭窄环后出现多个胆管口分离,需做多口的胆管-空肠内引流,该方法胆管口径小手术操作难度较大、多个吻合口增加吻合口漏的风险[20]。我院针对肝内相邻胆管狭窄、胆管切开后吻合困难的问题,创新性的提出“肝胆管内吻合”概念,具体操作要点:对于二级、三级胆管,存在相邻胆管狭窄时,采用5#薇乔线间断缝合相近的胆管后壁,延两胆管后壁之间纵行切开胆管壁,解除狭窄、减少出血,同时又保持胆管后壁的连续性,最后将肝门部胆管外壁进行拼合,形成肝胆管盆。该方法能有效解除高位的胆道梗阻,同时避免形成多个单独的胆管开口,降低手术吻合的难度。
总之,对于复杂肝胆管结石,往往因病程长、多次手术、结石复发率高、手术难度大等特点,一直是胆道外科治疗的难点。经皮经肝内镜(percutaneous transhepatic endoscope,PTES)联合钬激光碎石、超声引导下经胃肝造瘘联合电液压碎石术等的应用为无法手术的患者提供新的途径[21-22]。在部分手术患者肝硬化严重、肝脏比例失调、肝门胆管高位狭窄等复杂情况下,采取肝方叶切除、肝门胆管高位劈开整形的手术方式,能最大限度的保留患者的有用肝脏,同时达到解除狭窄,通畅引流,减少结石复发的效果,值得推广。
[1] 董家鸿, 叶晟.我国肝胆管结石病治疗理念及模式的变迁[J].中国实用外科杂志, 2016, 36(3):261-263.doi:10.7504/CJPS.ISSN1005-2208.2016.03.02.Dong JH, Ye S.Evolution and development of philosophy and paradigm in treatment for hepatolithiasis[J].Chinese Journal of Practical Surgery, 2016, 36(3):261-263.doi:10.7504/CJPS.ISSN1005-2208.2016.03.02.
[2] Franzini T, Moura RN, Bonifácio P, et al.Complex biliary stones management: cholangioscopy versus papillary large balloon dilation - a randomized controlled trial[J].Endosc Int Open, 2018.6(2):E131-E138.doi: 10.1055/s-0043-122493.
[3] 吴金术, 刘昌军, 周海兰, 等.肝胆管结石并左肝肥大右肝萎缩的分型与手术治疗[J].中国现代手术学杂志, 2011, 15(1):2-4.Wu JS, Liu CJ, Zhou HL, et al.Classification and Surgical Treatment of Hepatolithiasis Accompany with Left Hepatic Hypertrophy and Right Hepatic Atrophy[J].Chinese Journal of Modern Operative Surgery, 2011, 15(1):2-4.
[4] 吴金术, 彭创, 谭正, 等.肝内胆管结石并肝萎缩肥大征32例的诊治[J].中华普通外科杂志, 2017, 32(10):839-842.doi:10.3760/cma.j.issn.1007-631X.2017.10.012.Wu JS, Peng C, Tan Z, et al.Diagnosis and treatment of intrahepatic stone complicated with atrophy-hypertrophy complex[J].Zhong Hua Pu Tong Wai Ke Za Zhi, 2017, 32(10):839-842.doi:10.3760/cma.j.issn.1007-631X.2017.10.012.
[5] Rai AA, Nazeer A, Luck NH.Frequency of gallstones and mean BMI in decompensated cirrhosis[J].Pan Afr Med J, 2018.30:123.doi: 10.11604/pamj.2018.30.123.12742.
[6] 王坚, 陈炜.胆肠吻合术在高位胆管狭窄治疗中应用[J].中国实用外科杂志, 2014, 34(10):921-924.doi:10.7504/CJPS.ISSN1005-2208.2014.10.06.Wang J, Chen W.Application of bilioenterostomy in the treatment of hilar bile duct stricture[J].Chinese Journal of Practical Surgery, 2014, 34(10):921-924.doi:10.7504/CJPS.ISSN1005-2208.2014.10.06.
[7] Jarufe N, Figueroa E, Muñoz C, et al.Anatomic hepatectomy as a definitive treatment for hepatolithiasis: a cohort study[J].HPB (Oxford), 2012, 14(9):604-610.doi: 10.1111/j.1477-2574.2012.00488.x.
[8] 李恩亮, 邬林泉, 袁荣发, 等.第二肝门附近复杂性肝胆管结石的外科处理[J].中国普通外科杂志, 2015, 24(8):1083-1087.doi:10.3978/j.issn.1005-6947.2015.08.005.Li EL, Wu LQ, Yuan RF, et al.Surgical management of complicated bile duct stones around second porta hepatis[J].Chinese Journal of General Surgery, 2015, 24(8):1083-1087.doi:10.3978/j.issn.1005-6947.2015.08.005.
[9] Kaneko J, Kawata K, Watanabe S, et al.Clinical characteristics and risk factors for stent-stone complex formation following biliary plastic stent placement in patients with common bile duct stones[J].J Hepatobiliary Pancreat Sci, 2018, 25(10):448-454.doi: 10.1002/jhbp.584.
[10] 陈长义.肝胆管结石患者胆肠吻合术后再手术原因分析与对策[J].中国普通外科杂志, 2014, 23(8):1138-1140.doi:10.7659/j.issn.1005-6947.2014.08.027.Chen CY.Reoperation after bilioenteric anastomosis for intraand extra-hepatic bile duct stones: analysis of causes and counter measures[J].Chinese Journal of General Surgery, 2014, 23(8):1138-1140.doi:10.7659/j.issn.1005-6947.2014.08.027.
[11] Yan S, Tejaswi S.Clinical impact of digital cholangioscopy in management of indeterminate biliary strictures and complex biliary stones: a single-center study[J].Ther Adv Gastrointest Endosc,2019, 12:2631774519853160.doi: 10.1177/2631774519853160.
[12] 吴兆平, 陈伟力, 方宁波, 等.经肝圆韧带裂入路精准肝切除术的临床应用[J].当代医学, 2019, 25(15):102-104.doi:10.3969/j.issn.1009-4393.2019.15.039.Wu ZP, Chen WL, Fang NB, et al.Clinical application of accurate hepatectomy through hepatic round ligament approach[J].Contemporary Medicine, 2019, 25(15):102-104.doi:10.3969/j.issn.1009-4393.2019.15.039.
[13] 沈盛, 巩子君, 刘厚宝.肝门入路治疗肝门部胆管狭窄的价值与评价[J].中国实用外科杂志, 2019, 39(2):143-145.doi:10.19538/j.cjps.issn1005-2208.2019.02.10.Shen S, Gong ZJ, Liu HB.Value and evaluation of hilar surgical approach in hilar biliary stricture[J].Chinese Journal of Practical Surgery, 2019, 39(2):143-145.doi:10.19538/j.cjps.issn1005-2208.2019.02.10.
[14] Enliang L, Rongshou W, Shidai S, et al.Simple resection of the lesion bile duct branch for treatment of regional hepatic bile duct stones[J].Medicine (Baltimore), 2017, 96(27):e7414.doi: 10.1097/MD.0000000000007414.
[15] Li EL, Yuan RF, Liao WJ, et al.Intrahepatic bile duct exploration lithotomy is a useful adjunctive hepatectomy method for bilateral primary hepatolithiasis: an eight-year experience at a single centre[J].BMC Surg, 2019, 19(1):16.doi: 10.1186/s12893-019-0480-1.
[16] Li EL, Feng Q, Yang QP, et al.Effectiveness of hepatic parenchyma lithotomy of hepatolithiasis: A single-center experience[J].Medicine (Baltimore), 2017, 96(10):e6134.doi:10.1097/MD.0000000000006134.
[17] 殷晓煜.肝切除在肝胆管结石治疗中的作用及地位[J].中国实用外科杂志, 2016, 36(3):278-280.doi:10.7504/CJPS.ISSN1005-2208.2016.03.06.Yin XY.The values and status of hepatectomy in the treatment of hepatolithiasis[J].Chinese Journal of Practical Surgery, 2016,36(3):278-280.doi:10.7504/CJPS.ISSN1005-2208.2016.03.06.
[18] 侯德智, 吴韬, 刘斌, 等.不同临床分型肝胆管结石病手术方式选择的分析[J].中国普通外科杂志, 2014, 23(8):1043-1048.doi:10.7659/j.issn.1005-6947.2014.08.006.Hou DZ, Wu T, Liu B, et al.Analysis of selection of surgical approaches for hepatolithiasis with different clinical classifications[J].Chinese Journal of General Surgery, 2014,23(8):1043-1048.doi:10.7659/j.issn.1005-6947.2014.08.006.
[19] 吴金术, 陈晨, 蔡翊, 等.对胆石病诊疗的几点意见及经验[J].中国现代医学杂志, 2014, 24(14):76-78.Wu JS, Chen C, Cai Y, et al.Clinical opinions and experiences in diagnosis and treatment of cholelithiasis[J].China Journal of Modern Medicine, 2014, 24(14):76-78.
[20] Bektaş H, Gürbulak B, Şahin ZD, et al.Multiple plastic biliary stent placement in the management of large and multiple choledochal stones: single center experience and review of the literature[J].Wideochir Inne Tech Maloinwazyjne, 2017, 12(3):231-237.doi:10.5114/wiitm.2017.69107.
[21] Mandai K, Uno K, Yasuda K.Endoscopic lithotripsy for right intrahepatic bile duct stone through endoscopic ultrasoundguided hepaticogastrostomy[J].Endoscopy, 2019, 51(2):E40-41.doi:10.1055/a-0800-8429.
[22] 魏晓平, 胡明道, 张翔, 等.经皮经肝内镜联合不同碎石方式精准治疗复杂肝胆管结石:附49例报告[J].中国普通外科杂志, 2018,27(2):150-155.doi:10.3978/j.issn.1005-6947.2018.02.003.Wei XP, Hu MD, Zhang X, et al.Percutaneous transhepatic endoscopy combined with different lithotripsy methods for precision treatment of complicated hepatolithiasis: a report of 49 cases[J].Chinese Journal of General Surgery, 2018, 27(2):150-155.doi:10.3978/j.issn.1005-6947.2018.02.003.
