直肠癌根治术中对于肠系膜下动脉(inferior mesenteric artery,IMA)及其分支的处理,主要有保留左结肠动脉(left colonic artery,LCA)的低位结扎和不保留LCA的高位结扎两种方式。对于选择哪种处理方式更有优势,尚没有一个明确的指南推荐。国内外学者既往多倾向于高位结扎[1-4]。但近年来,越来越多的文献报道,低位结扎处理IMA并行彻底的淋巴结清扫,在术中出血量、手术时间、清扫淋巴结数目与高位结扎组无明显差异,并且保留LCA能够保证近端肠管血供,降低吻合口瘘发生率[5-8]。在远期疗效上,低位结扎和高位结扎的术后5年无病生存率和总生存率差异无明显统计学意义[9-11]。
根据LCA、乙状结肠动脉(sigmoid artery,SA)和直肠上动脉(superior rectal artery,SRA)的关系,日本学者Murono等[12]将肠系膜下动脉分支分成4型:I型(直乙共干型),II型(左乙共干型),III型(全共干型),IV型(无左型)。有学者[13]报道,IMA的不同分支分型会影响术者对其结扎位置的判断,并与术后吻合口瘘等并发症相关。随着螺旋CT技术的发展,CT血管成像(computed tomography angiography,CTA)技术广泛应用于临床[14-15]。术前对腹部CT增强扫描后,应用CTA技术进行腹部血管三维重建,可以清晰显示肠系膜下动脉的分支,并测量LCA根部至IMA根部的长度及了解有无Riolan弓缺如[16]。本研究回顾性分析2018年1月—2019年12月安徽医科大学第三附属医院胃肠外科收治的50例直肠癌患者的临床病理资料,探讨在术前CTA指导下,精准低位结扎并D3淋巴结清扫在腹腔镜直肠前切除术中应用的可行性及安全性。
1 资料与方法
1.1 一般资料
采用回顾性描述性研究方法。收集50例进展期直肠癌患者的临床病理资料,其中男28例,女22例;年龄40~78岁,平均(63.5±4.6)岁;体质量指数(body mass index,BMI)19.1~25.8 kg/m2,平均(21.2±1.6)kg/m2;肿瘤距离肛缘4.0~12.0 cm,平均(8.3±1.2)cm;行末端回肠预防性造瘘术8例。
1.2 纳入标准和排除标准
纳入标准:术前病理证实为直肠癌,且无远处转移;术前均行腹部CT增强扫描并下腹部血管三维重建,典型病例图片见图1;能够耐受腹腔镜手术;临床病理资料完整。排除标准:术中操作未严格遵守TME原则,致直肠系膜破损;既往存在腹部手术史;术前行放化疗。
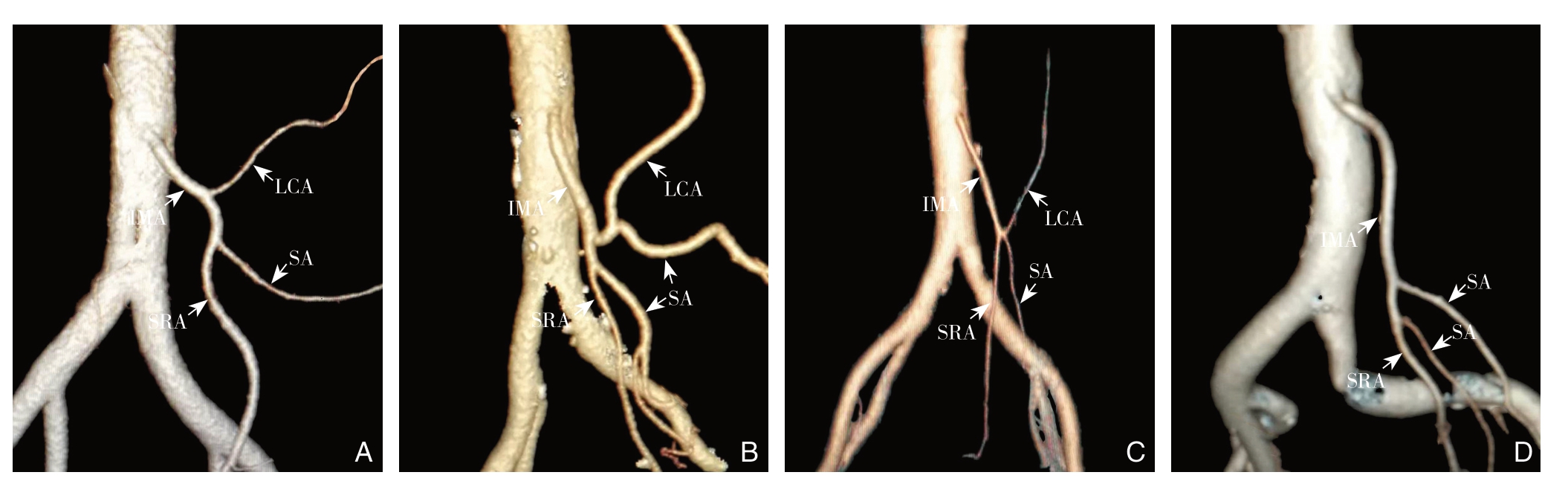
图1 IMA的分支分型的CT血管重建图片 A:I型;B:II型;C:III型;D:IV型
Figure1 CT vascular reconstruction of the branches of IMA A:Type I;B:Type II;C:Type III;D:Type IV
1.3 术前腹盆腔增强CT扫描方法及图像后处理
CT检查方法和图像处理:检查前口服复方聚乙二醇电解质散或甘露醇清洁肠道,空腹8 h。所有患者采用一台西门子公司640层螺旋CT进行平扫+增强扫描。造影剂采用非离子型对比剂碘克沙醇(100 mg/瓶,江苏恒瑞医药公司)。图像传送至PACS系统(Hwatech HiNet Picture Aechivina And Communication System 5.0,China)。图像后处理:医学影像三维重建工作站(Vitrea 6.3,Vital Images,Inc.Minnetonka,US),通过容积再现方式(volume rendering,VR)及多平面重建技术(multi-planar reconstruction,MPR),对IMA进行三维重建。
1.4 中间入路行保留LCA并D3淋巴结清扫手术
由同一组医师团队行腹腔镜辅助直肠前切除术,术中D3淋巴结清扫均由同一术者施行。患者取改良截石位,头低足高,右侧倾斜。五孔法穿刺置入腹腔镜器械。具体手术步骤包括:⑴第一助手将直肠乙状结肠系膜向腹侧及外侧牵拉绷紧,切开直肠乙状结肠右侧腹膜向上达IMA根部,注意勿损伤十二指肠(图2A);⑵ 术者左手牵拉切开的结肠系膜,超声刀游离已经打开的左侧Toldt间隙,并向外侧、头侧、尾侧扩展,注意显露和保护左侧输尿管和生殖血管,外侧达Monk白线(黄白交界线),头侧达肠系膜下静脉(inferior mesenteric vein,IMV)根部水平(图2B);⑶ 充分裸化IMA根部,注意防止肠系膜下神经从的损伤,采用“削铅笔”法,将动脉表面的脂肪组织剔除干净(图2C);⑷ 显露IMA各分支,确认LCA,清扫No.253淋巴结(图2D);⑸ 于LCA根部远侧切断IMA(图2E);⑹ 沿IMV右侧向头侧延长切开,裸化LCA并游离IMV(图2F);⑺ 在IMV和LCA交叉处切断IMV(图2G);⑻ No.253淋巴结清扫完成,相关血管处理完毕(图2H);⑼ 后续手术操作过程同传统腹腔镜辅助直肠前切除术(图2I)。

图2 保留LCA并D3淋巴结清扫的腹腔镜直肠前切除术 A:切开右侧直肠乙状结肠系膜;B:拓展Toldt 间隙;C:裸化IMA根部,注意防止肠系膜下神经丛的损伤;D:确认显露LCA,清扫No.253淋巴结;E:于LCA 远侧切断IMA;F:沿IMV 右侧向头侧延长切开;G:在IMV和LCA 交叉处切断IMV;H:No.253淋巴结清扫完成状态;I:大体标本
Figure2 Laparoscopic anterior resection of rectal cancer with LCA preservation and D3 lymphadenectomy A:Incision of the right rectosigmoid mesenteries;B:Extension of Toldt's space;C:Baring the root of the IMA,with caution of the injury of inferior mesenteric nerve plexus;D:Identification and exposure of IMA,and clearance of the No.253 lymph nodes;E:Division of the IMA in the distal end of LCA;F:Cranial incision along the right side of IMA;G:Division of IMA at the junction of IMV and LCA;H:Completion of No.253 lymph node dissection;I:Gross specimen
1.5 手术质量控制标准
上段直肠癌采用肿瘤特异性直肠系膜切除术(tumor-specific mesorectal excision,TSME),中下段直肠癌采用标准全直肠系膜切除术(total mesorectal excision,TME)。手术严格遵守TME原则:⑴ 锐性解剖盆筋膜壁层和脏层之间的无血管平面,保证切除标本的直肠系膜完整无破损;⑵ 肿瘤远端直肠系膜切除不少于5.0 cm或行TME;⑶ 对于中低位直肠癌应切除肿瘤远端肠管≥2.0 cm,对于超低位直肠癌,远切缘距离肿瘤 1 cm亦可行,但需术中冷冻切片病理报告确保切缘阴性。
1.6 观察指标
观察患者No.253淋巴结清扫时间、No.253淋巴结清扫数目、总手术时间、淋巴结清扫总数、术中出血量、肿瘤组织学分型、pTNM分期、术后住院时间、术后并发症(吻合口瘘、吻合口出血等)和随访情况。
1.7 数据处理
应用SPSS 16.0统计软件进行分析。正态分布的计量资料以均数±标准差( ±s)表示。计数资料以率表示。
±s)表示。计数资料以率表示。
2 结 果
2.1 IMA 血管分支分型情况
50例直肠癌患者中,IMA分支I-I V型所占比例分别为48.0%(24/50)、16.0%(8/50)、34.0%(17/50)和2.0%(1/50)。IMA长度为1.6~4.8 cm,平均(3.7±0.5)cm。Riolan弓缺如率70.0%(35/50)。
2.2 手术及术后情况
全组50例直肠癌患者,手术经过顺利,无中转开腹病例。No.253淋巴结清扫时间12~35 min,平均(18.5±5.8)min;No.253淋巴结清扫数量0~6枚,平均(4.5±1.3)枚,其中淋巴结阳性者2例,No.253淋巴结转移率4.0%(2/50),2例No.253阳性患者,术后病理分期均为III C期。全组患者总手术时间115~190min,平均(130±26)min;术中出血量30~150 mL,平均(65.8±7.8)mL;淋巴结清扫总数10~39枚,平均(17.6±4.5)枚。50例患者肿瘤组织学分型:高分化腺癌10例,中分化腺癌25例,低分化腺癌15例。pTNM分期:I期5例,IIB期23例,IIIA期15例,IIIB期5例,IIIC期2例。50例患者术后住院时间为8~15(12.5±2.3)d。50例患者术后均无吻合口瘘等严重并发症发生,1例术后解暗红色血便,给予止血治疗后好转。全组患者均痊愈出院。全组患者均获得随访,随访时间为3~26个月,其中1例术后病理分期为IIIC期且No.253淋巴结阳性患者,术后14个月出现肝脏转移。全组无死亡病例。
3 讨 论
3.1 保留LCA在腹腔镜下直肠癌根治术的临床意义
保留LCA在直肠癌根治术中可使近端结肠获得更好的血供,从而可有效预防吻合口瘘的发生。Komen等[17]在术中采用多普勒超声检测IMA根部结扎前后结肠残端血流灌注情况,发现结扎IMA,其供血分数明显减少。Tsujinaka等[18]在一项回顾性研究中发现,高位结扎组302例患者中有6例出现近端结肠坏死,而低位结扎组则无1例出现此并发症。尤小兰等[19]将136例直肠癌患者分为高位结扎组和低位结扎组,结果发现高位结扎组患者有7例发生吻合口瘘,9例存在不同程度的吻合口狭窄,低位结扎组分别仅有1例和2例,差异有统计学意义。国内其他学者的研究也获得了类似的结果[20-22]。此外,研究[23-24]表明保留左结肠动脉还有助于改善直肠癌患者术后排便功能,减少因神经损伤导致的排尿及性功能障碍。
3.2 术前行CT 增强扫描并血管重建的重要意义
部分学者[19,25]认为,IMA分支存在变异,保留LCA的根部淋巴结清扫,会增加操作难度,明显延长手术时间。术中如何显露并裸化IMA及其各分支,精准保留LCA并彻底清扫根部淋巴结,是既往低位结扎手术操作难点所在。利用CTA技术,对下腹部血管进行三维重建,可获知IMA分支分型、长度及Riolan弓缺如情况。因此,在CTA技术的指导下,行保留LCA的D3淋巴结清扫,较以往更加安全、可靠,且更加精准,并可明显缩短裸化血管时间,降低误扎血管和淋巴结残留的几率。本研究50例直肠癌患者,根据术前CT血管成像,提前获知IMA分支分型,术中均顺利显露IMA及其各分支,No.253淋巴结清扫满意且均未出现血管损伤、误扎血管等严重并发症。
黄俊等[13]在一项关于低位结扎组和高位结扎组的对照研究中发现,116例患者术后出现吻合口瘘8例,其中7例系IMA III型,且Riolan弓缺如并行IMA高位结扎。多因素回归分析显示,IMA III型和Riolan弓缺如是吻合口瘘发生的独立危险因素。这项研究成果也证明了术前通过CT血管成像确认IMA分支分型及Riolan弓有无缺如的意义所在。本研究中,有5例患者系IMA III型并Riolan弓缺如,术者均给予行IMA低位结扎,结果无1例出现吻合口瘘。
3.3 保留LCA并D3淋巴结清扫的技术要点
腹腔镜直肠前切除术,所谓的“第一刀”非常重要,如果手术一开始即进入错误的层面,可能导致出血或者损伤输尿管、生殖血管等,甚至使手术无法继续进行。笔者的常规操作是,第一助手将直肠乙状结肠系膜向腹侧及外侧牵拉绷紧后,术者用抓钳探测骶骨岬,确定腹主动脉分叉处的尾侧。仔细观察骶骨岬与腹主动脉分叉处中间部位的乙状结肠系膜,超声刀切开系膜并将切除线向骨盆方向稍微延续。此时,腹膜切开的要尽可能薄一些,同时需要注意骨盆方向的切除线可能会与设想有一定的偏差。接下来,助手将直肠向腹侧牵拉,术者在直肠的背侧进行钝性分离,最终进入到疏松组织中去,即进入了直肠后间隙中。确认直肠固有筋膜后,转向头侧方向,沿直肠固有筋膜向上游离延续的左侧Toldt融合筋膜。采用上述方法,可以很容易进入正确的层面,即位于左侧Toldt融合筋膜和Gerota筋膜之间的Toldt间隙。郑民华等[26-28]国内学者认为采用头侧中间入路,从IMA头侧的腹主动脉表面腹膜处打开进入左侧Toldt间隙较传统入路更容易一些。不管采用何种入路,具有扎实的临床解剖学知识,才是避免进入错误层面的关键。
一旦通过正确层面找到IMA根部,即可切开血管鞘,在血管外膜表面采用“削铅笔法”向远侧清扫,将动脉表面的淋巴脂肪组织剔除干净。也可以在血管鞘外清扫淋巴结,这样可以保留血管鞘表面的神经纤维,但鞘外清扫容易出血,清扫过程中应注意止血。根据术前CT血管成像,了解IMA的长度和各分支的大致位置,超声刀小口钳夹组织并激发,采用“小步快跑”法清扫血管周围脂肪淋巴组织,并逐步显露IMA各分支,确认LCA,清扫No.253淋巴结。清扫范围:肠系膜下动脉起始部为头侧缘,肠系膜下静脉右侧为外侧缘,左结肠动脉根部为足侧缘,肠系膜下动脉左侧为内侧缘[29]。清扫的NO.253淋巴结单独送检,也可以向左侧绕过LCA和结肠系膜整块切除(enbloc)。于LCA根部远侧切断IMA。沿IMV右侧向头侧延长切开,裸化LCA并游离IMV,LCA和IMV一般伴行一段距离,注意清扫它们之间的组织。关于IMV的切断位置还存在争议,笔者常规的做法是在IMV和LCA交叉处切断IMV。李心翔等[30]提出了“肠系膜下动脉三角区域淋巴结”这一新概念,如果将这一区域淋巴结清扫干净,即能够达到肿瘤学根治目的。
综上所述,对所有直肠癌患者,建议术前均行常规腹盆腔CT增强扫描并进行血管三维重建。在CTA技术指导下,精准低位结扎并D3淋巴结清扫的腹腔镜直肠前切除术安全可行,应向广大胃肠外科医生推广应用。
[1]Hida J,Okuno K.High ligation of the inferior mesenteric artery in rectal cancer surgery[J].Surg Today,2013,43(1):8-19.doi:10.1007/s00595-012-0359-6.
[2]陈仕才,宋新明,陈志辉,等.肠系膜下动脉结扎方式对乙状结肠癌和直肠癌患者预后影响的Meta分析[J].中华胃肠外科杂志,2010,13(9):674-677.doi:10.3760/cma.j.issn.1671-0274.2010.09.013.
Chen SC,Song XM,Chen ZH,et al.Role of different ligation of the inferior mesenteric artery in sigmoid colon or rectal cancer surgery:a meta-analysis[J].Chinese Journal of Gastrointestinal Surgery,2010,13(9):674-677.doi:10.3760/cma.j.issn.1671-0274.2010.09.013.
[3]Kanemitsu Y,Hirai T,Komori K,et al.Survival benefit of high ligation of the inferior mesenteric artery in sigmoid colon or rectal cancer surgery[J].Br J Surg,2006,93(5):609-615.doi:10.1002/bjs.5327.
[4]Singh D,Luo J,Liu XT,et al.The long-term survival benefits of high and low ligation of inferior mesenteric artery in colorectal cancer surgery:A review and meta-analysis[J].Medicine (Baltimore),2017,96(47):e8520.doi:10.1097/MD.0000000000008520.
[5]牛晋卫,宁武,王文跃,等.保留左结肠动脉在腹腔镜下直肠癌前切除术中的临床作用[J].中华医学杂志,2016,96(44):3582-3585.doi:10.3760/cma.j.issn.0376-2491.2016.44.010.
Niu JW,Ning W,Wang WY,et al.Clinical effect of preservation of the left colonic artery in laparoscopic anterior resection for rectal cancer[J].National Medical Journal of China,2016,96(44):3582-3585.doi:10.3760/cma.j.issn.0376-2491.2016.44.010.
[6]孙跃明,封益飞,唐俊伟,等.保留左结肠动脉腹腔镜全直肠系膜切除术治疗中低位直肠癌的临床疗效[J].中华消化外科杂志,2019,18(5):478-483.doi:10.3760/cma.j.issn.1673-9752.2019.05.014.
Sun YM,Feng YF,Tang JW,et al.Clinical effects of laparoscopic left colic artery-preserving total mesorectal excison for middlelow rectal cancer[J].Chinese Journal of Digestive Surgery,2019,18(5):478-483.doi:10.3760/cma.j.issn.1673-9752.2019.05.014.
[7]张明府,吴永丰,柳东.腹腔镜直肠癌前切除术中保留左结肠动脉对术后吻合口漏及近期疗效的影响[J].临床外科杂志,2019,27(5):400-404.doi:10.3969/j.issn.1005-6483.2019.05.014.
Zhang MF,Wu YF,Liu D.Influence of preserving left colic artery during during laparoscopic anterior resection for rectal cancer on anastomotic leakage and recent efficacy[J].Journal of Clinical Surgery,2019,27(5):400-404.doi:10.3969/j.issn.1005-6483.2019.05.014.
[8]张鲁阳,臧潞,马君俊,等.腹腔镜直肠癌根治术中保留左结肠动脉的临床意义[J].中华胃肠外科杂志,2016,19(8):886-891.doi:10.3760/cma.j.issn.1671-0274.2016.08.018.
Zhang LY,Zang L,Ma JJ,et al.Preservation of left colic artery in laparoscopic radical operation for rectal cancer[J].Chinese Journal of Gastrointestinal Surgery,2016,19(8):886-891.doi:10.3760/cma.j.issn.1671-0274.2016.08.018.
[9]Cirocchi R,Trastulli S,Farinella E,et al.High tie versus low tie of the inferior mesenteric artery in colorectal cancer:a RCT is needed[J].Surg Oncol,2012,21(3):e111-123.doi:10.1016/j.suronc.2012.04.004.
[10]沈荐,李敏哲,杜燕夫,等.保留左结肠动脉的腹腔镜直肠癌低位前切除术的长期疗效分析[J].中华胃肠外科杂志,2017,20(6):660-664.doi:10.3760/cma.j.issn.1671-0274.2017.06.014.
Shen J,Li MZ,Du YF,et al.Long-term outcomes of laparoscopic low anterior resection of rectal carcinoma with preservation of the left colic artery[J].Chinese Journal of Gastrointestinal Surgery,2017,20(6):660-664.doi:10.3760/cma.j.issn.1671-0274.2017.06.014.
[11]Yand Y,Wang G,He J,et al.High tie versus low tie of inferior mesenteric artery in colorectal cancer:A meta-analysis[J].Int J Surg,2018,52:20-24.doi:10.1016/j.ijsu.2017.12.030.
[12]Murono K,Kawai K,Kazama S,et al.Anatomy of the inferior mesenteric artery evaluated using 3-dimensional CT angiography[J].Dis Colon Rectum,2015,58(2):214-219.doi:10.1097/DCR.0000000000000285.
[13]黄俊,周家铭,万英杰,等.肠系膜下动脉血管分型及Riolan动脉弓缺如对腹腔镜直肠癌根治术后吻合口瘘发生率的影响[J].中华胃肠外科杂志,2016,19(10):1113-1118.doi:10.3760/cma.j.issn.1671-0274.2016.10.008.
Huang J,Zhou JM,Wan YJ,et al.Influences of inferior mesenteric artery types and Riolan artery arcade absence on the incidence of anastomotic leakage after laparoscopic resection of rectal cancer[J].Chinese Journal of Gastrointestinal Surgery,2016,19(10):1113-1118.doi:10.3760/cma.j.issn.1671-0274.2016.10.008.
[14]李晨霞,张蕴,张月浪,等.64层螺旋CT血管成像在肠系膜血管缺血性疾病中的临床价值[J].实用放射学杂志,2014,30(2):250-253.doi:10.3969/j.issn.1002-1671.2014.02.014.
Li CX,Zhang Y,Zhang YL,et al.Clinical value of 64-slice spiral CT in the mesenteric vascular ischemic disease[J].Journal of Practical Radiology,2014,30(2):250-253.doi:10.3969/j.issn.1002-1671.2014.02.014.
[15]曹建新,王一民,张羽,等.联合应用低管电压和对比剂个体化方案进行腹部CT血管成像的研究[J].中华放射学杂志,2012,46(10):902-906.doi:10.3760/cma.j.issn.1005-1201.2012.10.007.
Cao JX,Wang YM,Zhang Y,et al.Study of abdominal CT angiography in low tube voltage setting combined with personalized contrast media application[J].Chinese Journal of Radiology,2012,46(10):902-906.doi:10.3760/cma.j.issn.1005-1201.2012.10.007.
[16]丁元升,田相安,孙钦立,等.双源螺旋CT血管成像在保留左结肠动脉的3D腹腔镜下直肠癌根治术中的应用研究[J].影像研究与医学应用,2018,2(8):59-62.
Ding YS,Tian XA,Sun QL,et al.Application of dual-source CT angiography in 3D laparoscopic radical resection of rectal cancer with preservation of left colonic artery[J].Journal of Imaging Research and Medical Applications,2018,2(8):59-62.
[17]Komen N,Slieker J,de Kort P,et al.High tie versus low tie in rectal surgery:comparison of anastomotic perfusion[J].Int J Colorectal Dis,2011,26(8):1075-1078.doi:10.1007/s00384-011-1188-6.
[18]Tsujinaka S,Kawamura YJ,Tan KY,et al.Proximal bowel necrosis after high ligation of the inferior mesenteric artery in colorectal surgery[J].Scand J Surg,2012,101(1):21-25.doi:10.1177/145749691210100105.
[19]尤小兰,王元杰,程之逸,等.腹腔镜直肠癌全直肠系膜切除术中保留左结肠动脉的临床研究[J].中华胃肠外科杂志,2017,20(10):1162-1167.doi:10.3760/cma.j.issn.1671-0274.2017.10.016.
You XL,Wang YJ,Cheng ZY,et al.Clinical study of preserving left colic artery during laparoscopic total mesorectal excision for the treatment of rectal cancer[J].Chinese Journal of Gastrointestinal Surgery,2017,20(10):1162-1167.doi:10.3760/cma.j.issn.1671-0274.2017.10.016.
[20]吴传福,钱正海,郎建华,等.肠系膜下动脉在腹腔镜直肠癌根治术中的处理方式 及保留左结肠动脉的临床意义[J].腹腔镜外科杂志,2019,24(4):267-270.doi:10.13499/j.cnki.fqjwkzz.2019.04.267.
Wu CF,Qian ZH,Lang JH,et al.Treatment of the inferior mesenteric artery in laparoscopic radical resection of rectal cancer and the clinical significance of reservation the left colonic artery[J].Journal of Laparoscopic Surgery,2019,24(4):267-270.doi:10.13499/j.cnki.fqjwkzz.2019.04.267.
[21]成军,周玲,陈涛,等.保留左结肠动脉的腹腔镜低位直肠癌前切除术[J].中国微创外科杂志,2017,17(9):780-782.doi:10.3969/j.issn.1009-6604.2017.09.005.
Cheng J,Zhou L,Chen T,et al.Effect on Preservation of the Left Colonic Artery in Laparoscopic Anterior Resection of Low Rectal Carcinoma[J].Chinese Journal of Minimally Invasive Surgery,2017,17(9):780-782.doi:10.3969/j.issn.1009-6604.2017.09.005.
[22]滕文浩,魏丞,刘文居,等.保留左结肠动脉对接受新辅助治疗的直肠癌患者术后吻合口漏的影响[J].中华胃肠外科杂志,2019,22(6):566-572.doi:10.3760/cma.j.issn.1671-0274.2019.06.010.
Teng WH,Wei C,Liu WJ,et al.Effect of preservation of left colic artery on postoperative anastomotic leakage of patients with rectal cancer after neoadjuvant therapy[J].Chinese Journal of Gastrointestinal Surgery,2019,22(6):566-572.doi:10.3760/cma.j.issn.1671-0274.2019.06.010.
[23]谯瞧,车向明,樊林.直肠癌腹腔镜全直肠系膜切除术对排尿功能的影响研究[J].中国普通外科杂志,2015,24(10):1427-1432.doi:10.3978/j.issn.1005-6947.2015.10.016.
Qiao Q,Chen XM,Fan L.Analysis of impact of laparoscopic total mesorectal excision on urinary function[J].Chinese Journal of General Surgery,2015,24(10):1427-1432.doi:10.3978/j.issn.1005-6947.2015.10.016.
[24]屈景辉,贺佳蓓,张琦,等.保留左结肠动脉在腹腔镜直肠癌前切除术中的临床应用[J].实用医学杂志,2018,34(17):2900-2903.doi:10.3969/j.issn.1006-5725.2018.17.020.
Qu JH,He JB,Zhang Q,et al.Clinical application of preservation of the left colonic artery in laparoscopic anterior resection for rectal cancer[J].The Journal of Practical Medicine,2018,34(17):2900-2903.doi:10.3969/j.issn.1006-5725.2018.17.020.
[25]任龙,张云,沈正海.腹腔镜直肠癌前切除术中保留左结肠动脉与否的Meta分析[J].中华普通外科学文献:电子版,2018,12(5):367-372.doi:10.3877/cma.j.issn.1674-0793.2018.05.020.
Ren L,Zhang Y,Shen ZH.Preservation of left colon artery or not in laparoscopic anterior resection of rectal cancer:A Meta-analysis[J].Chinese Archives of General Surgery:Electronic Edition,2018,12(5):367-372.doi:10.3877/cma.j.issn.1674-0793.2018.05.020.
[26]郑民华,马君俊,臧潞,等.头侧中间入路腹腔镜直肠癌根治手术[J].中华胃肠外科杂志,2015,18(8):835-836.doi:10.3760/cma.j.issn.1671-0274.2015.08.030.
Zheng MH,Ma JJ,Zang L,et al.Laparoscopic radical resection for rectal cancer via central approach[J].Chinese Journal of Gastrointestinal Surgery,2015,18(8):835-836.doi:10.3760/cma.j.issn.1671-0274.2015.08.030.
[27]马君俊,洪希周,臧潞,等.头侧中间入路与传统中间入路腹腔镜直肠癌根治术的疗效分析[J].中华消化外科杂志,2016,15(8):780-784.doi:10.3760/cma.j.issn.1673-9752.2016.08.005.
Ma JJ,Hong XZ,Zang L,et al.Effect analysis of cephalomedial to lateral and traditional medial-to-lateral approaches for laparoscopic radical resection of rectal cancer[J].Chinese Journal of Digestive Surgery,2016,15(8):780-784.doi:10.3760/cma.j.issn.1673-9752.2016.08.005.
[28]康博雄,夏博伟,樊勇,等.腹腔镜下头侧中间入路在保留左结肠动脉的Dixon手术中的应用(附22例报告)[J].中国微创外科杂志,2017,17(10):897-898.doi:10.3969/j.issn.1009-6604.2017.10.009.
Kang BX,Xia BW,Fan Y,et al.Application of Head-medial Approach in Laparoscopic Anterior Resection of Rectal Carcinoma with Preservation of the Left Colonic Artery:Report of 22 Cases[J].Chinese Journal of Minimally Invasive Surgery,2017,17(10):897-898.doi:10.3969/j.issn.1009-6604.2017.10.009.
[29]渡边昌彦,上西纪夫,後藤溝一,等.小肠结肠外科手术操作要领及技巧[M].张雪峰,金红旭,译.北京:人民卫生出版社,2012:82.
Masahiko W,Takao U,Mizogo G,et al.Essential points and skills of operation in small intestinal and colonic surgery[M].Zhang XF,Jin HX,translate.Beijing:People's Medical Publishing House,2012:82.
[30]李心翔,李清国.腹腔镜直肠癌术中左结肠动脉保留的意义[J].中华胃肠外科杂志,2018,21(3):272-275.doi:10.3760/cma.j.issn.1671-0274.2018.03.006.
Li XX,Li QG.Significance of the preservation of left colic artery in laparoscopic resection of rectal cancer[J].Chinese Journal of Gastrointestinal Surgery,2018,21(3):272-275.doi:10.3760/cma.j.issn.1671-0274.2018.03.006.
