随着腔内技术不断发展,胸主动脉腔内修复术(thoracic endovascular aortic repair,TEVAR)已广泛应用于临床[1-3],而主动脉弓部疾病的腔内治疗仍然是一个巨大挑战,通过分支血管重建来延长近端正常锚定区是治疗主动脉弓部疾病的关键[4]。分支重建方法包括平行支架技术、分支支架技术、体外开窗及开槽技术、原位开窗技术、杂交手术等,本中心对体外开窗及开槽技术进行了探讨,现报告如下。
1 资料与方法
1.1 一般资料
收集海南省人民医院血管外科2016年9月—2019年4月共23例主动脉弓部疾病患者的临床资料,其中14例B型主动脉夹层,7例胸主动脉瘤,2例穿透性溃疡,均接受TEVAR并重建弓上分支血管。患者基本临床资料见表1。
所有患者术前均行主动脉至双侧股动脉CT血管成像(computed tomography angiography,CTA),入选标准:动脉夹层近端锚定区距分支血管<10~15 mm[5];主动脉瘤近端锚定区距分支血管<20 mm[6];病变累及弓部或锚定区弯曲度过大。排除标准:近端锚定区直径>42 mm;病变累及弓部大弯侧;入路血管闭塞;难以耐受手术者。
1.2 器材准备
体外支架移植物开槽及开窗处理:⑴后撤输送系统外鞘,使拟开窗部分处于完全展开状态;⑵根据术前测量结果用标记笔进行定位、剪裁,0.014英寸导丝镶边并用5-0 Prolene缝线固定;⑶应用操纵杆原有标记或在操纵杆重新做标记,该标记与支架Mark“8”处于同一条直线上;⑷用丝线捆绑支架,通过旋转操纵杆将支架缓慢、完全回装至输送系统;⑸将支架推送器朝操纵杆标记的反方向进行预弯,使推送器在自然状态下呈45~60°弯曲。
表1 23例患者基本资料
Table 1 General data of the 23 patients
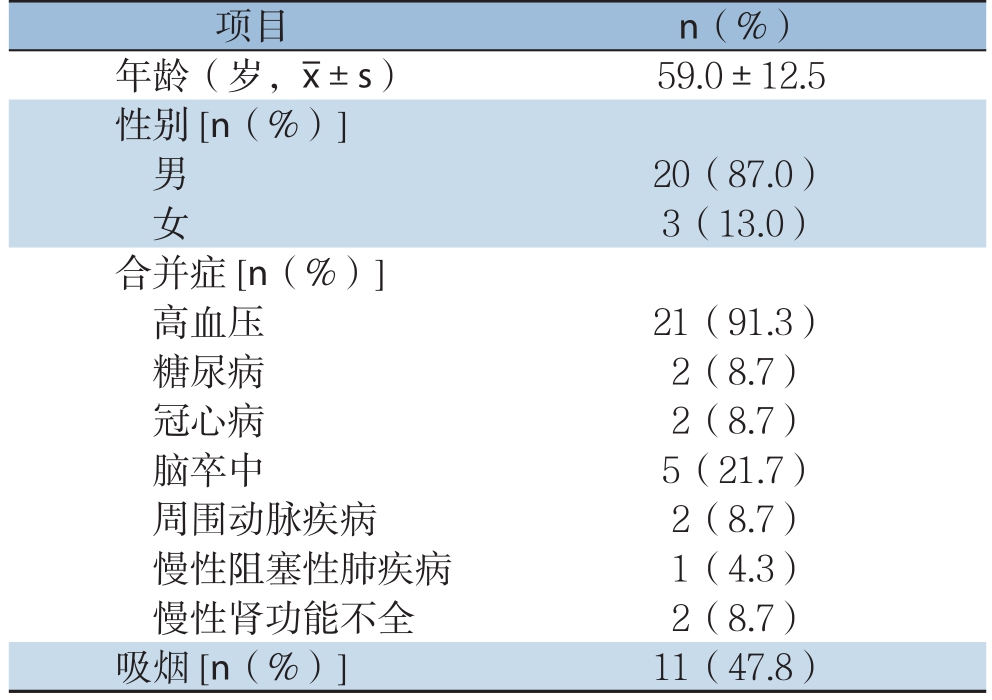
项目 n(%)年龄(岁,x±s) 59.0±12.5性别[n(%)]男20(87.0)女3(13.0)合并症[n(%)]高血压 21(91.3)糖尿病 2(8.7)冠心病 2(8.7)脑卒中 5(21.7)周围动脉疾病 2(8.7)慢性阻塞性肺疾病 1(4.3)慢性肾功能不全 2(8.7)吸烟[n(%)] 11(47.8)
1.3 手术方法
在预计重建的分支血管预置导丝至升主动脉,从左锁骨下动脉(LSA)置入5 F猪尾巴导管于升主动脉备造影用。股动脉预埋2根Proglide缝线后置入5 F鞘,从股动脉置入5 F猪尾巴导管于升主动脉,调整至主动脉弓切线位造影,明确病变位置及形态。全身肝素化(75 U/kg),从股动脉置入Lunderquist导丝于升主动脉,输送系统的操纵杆标记始终朝向患者背侧,即6点方向,由助手固定操纵杆,支架沿Lunderquist导丝缓慢推送至病变区域。收缩压降至90 mmHg(1 mmHg=0.133 kPa),释放支架2~3节后造影,根据造影结果沿主动脉纵轴方向调整支架位置,调整后快速释放支架(图1-3)。再次造影,若分支血管通畅,根据开窗位置和分支血管开口对合情况选择性放置分支支架;若分支血管被遮盖,根据具体情况选择原位开窗、烟囱支架或随访观察。穿刺点压迫止血,送回病房。
1.4 术后处理
术后7 d与3、6个月及每年复查CTA,了解主体支架、分支支架通畅情况及有无内漏,根据具体情况制定相应治疗方案。

图1 主动脉弓部动脉瘤并附壁血栓 A:计划LSA预开窗;B:体外开窗;C:术中沿主动脉纵轴方向调整支架位置;D:术后复查弓部动脉瘤消失,分支血管通畅,无内漏
Figure 1 Aortic arch aneurysm with mural thrombus A:Pre-fenestration to reconstruct LSA;B:In-vitro fenestration;C:Adjusting stent position along longitudinal axis of the aorta;D:Disappearance of arch aneurysm,patent branch vessels and on endoleak after operation

图2 慢性B型主动脉夹层 A:计划LSA预开窗;B:破口位于弓部小弯侧(箭头所示),术中对位准确,不放置分支支架;C:术后复查LSA显影好,无内漏;D:术后3个月复查支架无移位,LSA显影好,无内漏
Figure 2 Chronic type B aortic dissection A:Pre-fenestration to reconstruct LSA;B:The break located at the lesser curvature side of the arch(shown by arrow),accurate intraoperative alignment and no branch stent placement;C:Good display of LSA and no endoleak after operation;D:No stent displacement of,good LSA imaging and no endoleak at 3 months after operation
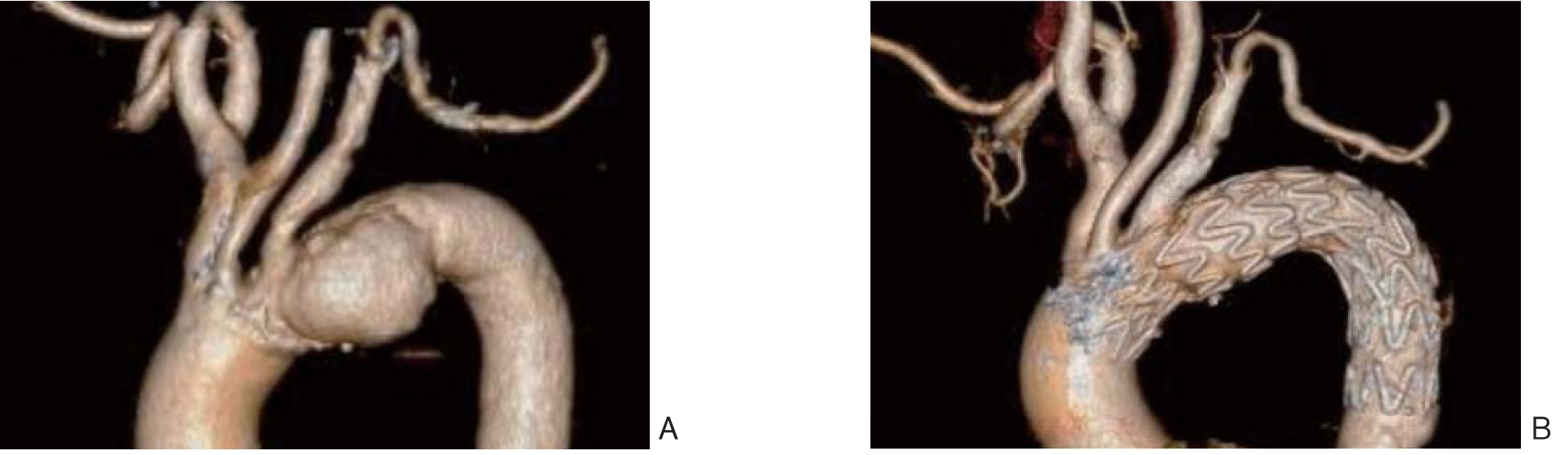
图3 主动脉弓部动脉瘤 A:计划无名动脉(IA)、左颈总动脉(LCCA)预开槽,LSA预开窗;B:术后复查弓部动脉瘤消失,分支血管通畅,无内漏
Figure 3 Aortic arch aneurysm A:Planning to reconstruct innominate artery(IA)and left common carotid artery(LCCA)by scallop an reconstruct LSA by fenestration;B:Disappearance of arch aneurysm,patent branch vessels and no endoleak after operation
2 结果
2.1 手术情况
支架近端放置Z0区3例,Z1区6例,Z2区14例;平均手术时间(122.8±53.5)min,支架近端平均直径(33.3±3.9)mm。重建弓上分支血管共40条,其中IA 3条,LCCA 9条,LSA 23条,迷走左椎动脉(ALVA)3条,迷走右锁骨下动脉(ARSA)2条(表2)。开槽技术重建15条,平均宽度18.6 mm,深度15.2 mm;开窗技术重建25条,窗口平均直径9.0 mm。共放置16枚分支支架,8例患者共10条分支血管开窗对位良好,未放置分支支架。
表2 手术相关资料
Table 2 The surgery-related variables
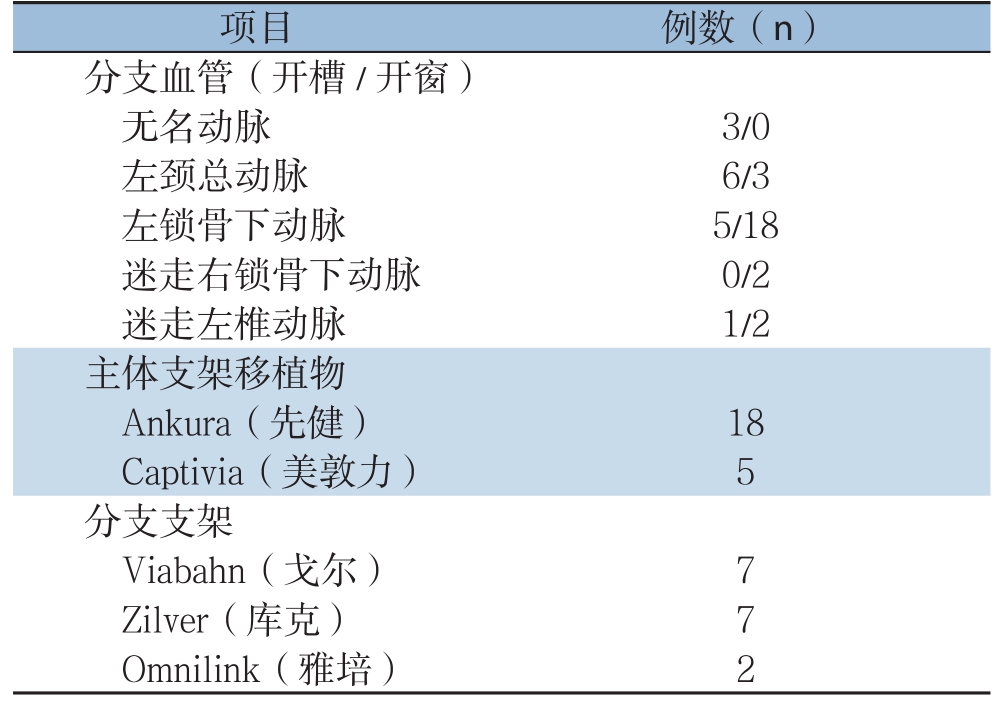
项目 例数(n)分支血管(开槽/开窗)无名动脉 3/0左颈总动脉 6/3左锁骨下动脉 5/18迷走右锁骨下动脉 0/2迷走左椎动脉 1/2主体支架移植物Ankura(先健) 18 Captivia(美敦力) 5分支支架Viabahn(戈尔) 7 Zilver(库克) 7 Omnilink(雅培) 2
2.2 并发症及随访
中位随访时间7.8(3~23)个月。40条分支血管中9条被遮盖,均为LSA,技术成功率77.5%,9条血管中6条采取烟囱支架术作为补救措施,2条经过评估可随访观察,1条为死亡病例。1例胸主动脉瘤患者既往有鼻咽癌史,术后3个月LSA烟囱支架血栓形成;4例患者出现内漏,3例为II型内漏,1例为I型内漏,其中2例内漏随访中消失,1例内漏减少,1例内漏尝试栓塞失败。31条分支血管术后通畅,随访中1条LSA术后3个月血栓形成,6条分支血管失访。围手术期出现2例缺血性脑卒中;1例急性B型夹层患者合并左肾梗死、肠缺血,急诊TEVAR术,术后第1天突发心脏骤停、死亡。无截瘫发生。
3 讨论
开放手术治疗主动脉弓部疾病创伤大、病死率高;杂交技术手术时间长、创伤较大,围术期脑卒中、内漏等并发症仍是难题;随着腔内技术快速发展,全腔内技术治疗主动脉弓部疾病已成为趋势[7-11]。主动脉弓部疾病仍然是一个巨大的挑战,如何隔绝病灶同时重建弓上分支是腔内治疗的重点。目前重建弓上分支主要有平行支架技术、分支支架技术、开窗技术等,其中平行支架技术操作相对简单,但容易发生内漏、分支支架受压导致狭窄或闭塞[12-14];分支支架技术主体稳定性强,能有效减少内漏发生,包括自制分支和商业化分支两种,自制分支适用于瘤体较大的真性动脉瘤,使其有足够空间重建、释放分支支架,商业化分支定制周期长、费用昂贵,难以广泛开展[15];开窗技术包括原位开窗和体外预开窗两种,体外预开窗技术需经过精准测量,能有效降低主动脉弓部疾病腔内治疗内漏发生率[16-17],且多中心的早期结果已证实该技术是安全有效[18-21]。
支架移植物的覆膜部分不仅能隔绝病灶,还能稳定支架的整体结构。大面积开槽可能出现镍钛合金相互嵌顿,导致支架无法正常释放,尤其是开槽后的回装过程可能出现人为造成支架嵌顿。本组中11例患者采用开槽技术重建15条分支血管,平均开槽宽度18.6 mm,深度15.2 mm,无支架嵌顿发生。为了降低嵌顿概率和避免支架移植物整体结构破坏,我中心经验:一是避免开槽面积过大,宽度和深度均<20 mm;二是波段尖端部分保留覆膜,避免尖端部分插入相邻波段;三是用丝线捆绑支架,一节一节回装,避免支架旋转;四是开槽前缘保留2~3 mm覆膜,以免支架小波段发散式变形。为了使支架更顺利翻转,需提前将输送系统进行预弯,预弯方向为开窗的反方向,预弯后的输送系统在自然状态下角度控制在45~60°,预弯后的输送系统更容易通过主动脉弓。预弯前将导丝置入输送系统,避免预弯时支架内鞘芯发生皱褶。为了窗口和分支血管准确对位,窗口边缘用0.014英寸导丝镶边并5-0 Prolene缝线固定或拆卸“8”字进行标记,亦可利用支架金属波段进行标记。
当支架进入主动脉弓部后,只能从主动脉纵轴方向来调整支架位置,而无法调整其钟点方向,因此,术前CT三维成像的精准测量和体外开窗设计尤其重要。支架释放过程中,助手必须确保操纵杆标记始终朝向6点方向,患者收缩压降至90 mmHg左右,释放2~3节大波段,分支血管与支架金属标记准确对位后逐步完全释放。本组共重建40条分支血管,其中9条对位不良,可能存在以下因素:一是主动脉弓扭曲,Mark“8”不能准确到达预定位置;二是支架移植物体外开窗后,回装过程中可能出现旋转,导致钟点方向的偏差;三是当开窗位置的支架周径与真实血管的周径不匹配时,可能出现对位不良;四是输送系统在前行过程中因血管扭曲而出现无法控制的旋转,建议使用同步性更好的推送器,如Captivia。提前在分支血管预置导丝,通过烟囱支架或原位开窗等补救方法能有效避免脑卒中发生。Yokoi等[22]提出重建LSA指征:⑴LSA通过左乳内动脉供血冠状循环;⑵左椎动脉为优势动脉;⑶有脊髓缺血风险。本组研究中9条分支血管被遮盖,均为LSA,其中2条随访观察,均无特殊。
当开窗位置准确对位后是否放置分支支架问题依然存在争议,一方面分支支架可以纠正开窗与分支血管开口之间的微小偏差,稳定大支架,防止远期支架移位[23-25];另一方面分支支架具有再狭窄、治疗费用高等缺点。Lala等[26]认为,对于腹主动脉开窗患者,分支支架释放组的分支血管远期通畅率高于未释放组。本组中8例患者共10条分支血管预开窗后未放置分支支架,随访分支血管通畅,无内漏。因此,笔者认为,当开窗准确对位后可以不放置分支支架,但需满足以下条件:⑴主体支架近端Oversize<5%;⑵病变位于小弯侧或弓部远端,窗口与分支血管开口贴合紧密;⑶开窗与分支血管开口对位准确,用4 F猪尾巴导管从分支血管多角度通过开窗,若导管无变形提示对位良好;⑷患者依从性好,术后严格控制血压,避免血压过高引起支架移植物移位。
综上所述,体外开窗及开槽技术能有效解决主动脉弓部疾病TEVAR术中重建分支血管所面临的难题,但该技术不能完全适用所有主动脉弓部疾病,需要综合考虑病变特征,选择合适病例,联合杂交技术、烟囱支架、原位开窗、分支支架等技术,降低围手术期患者并发症的发生率。
[1]刘昭,童垣皓,于同,等.3D打印引导下采用开窗或分支支架治疗胸腹主动脉疾病[J].中华普通外科杂志,2019,34(3):213-216.doi:10.3760/cma.j.issn.1007-631X.2019.03.006.Liu Z,Tong YH,Yu T,et al.Treatment of thoraco-abdominal aortic disease with fenestrated stent-graft or branch stent-graft technique guided by 3D printing[J].Zhong Hua Pu Tong Wai Ke Za Zhi,2019,34(3):213-216.doi:10.3760/cma.j.issn.1007-631X.2019.03.006.
[2]Wooster M,Zwiebel B,Back M,et al.Early Experience with Snorkels and Chimneys for Expanding the Indications for Use of Endovascular Aneurysm Repair[J].Ann Vasc Surg,2017,41:105-109.doi:10.1016/j.avsg.2016.09.037.
[3]依地热斯·艾山,李新喜,田野,等.开窗支架与烟囱技术腔内治疗腹主动脉瘤疗效比较的Meta分析[J].中国普通外科杂志,2019,28(6):696-705.doi:10.7659/j.issn.1005-6947.2019.06.008.Yidiresi·AS,Li XX,Tian Y,et al.Fenestrated endografts versus chimney stent repair for abdominal aortic aneurysms:a Metaanalysis[J].Chinese Journal of General Surgery,2019,28(6):696-705.doi:10.7659/j.issn.1005-6947.2019.06.008.
[4]Riambau V,Böckler D,Brunkwall J,et al.Editor's Choice-Management of Descending Thoracic Aorta Diseases:Clinical Practice Guidelines of the European Society for Vascular Surgery(ESVS)[J].Eur J Vasc Endovasc Surg,2017,53(1):4-52.doi:10.1016/j.ejvs.2016.06.005.
[5]陆清声,景在平.B型主动脉夹层腔内治疗技术要点以及应避免的误区[J].临床误诊误治,2014,27(3):4-6.doi:10.3969/j.issn.1002-3429.2014.03.002.Lu QS,Jing ZP.Essentials and Misunderstanding of Treatment Technology for Type B Aortic Dissection Endovascular[J].Clinical Misdiagnosis&Mistherapy,2014,27(3):4-6.doi:10.3969/j.issn.1002-3429.2014.03.002.
[6]Kondo S,Katada Y.Fenestrated Stent Graft Repair for Thoracic Aortic Aneurysm[J].Kyobu Geka,2016,69(8):638-643.
[7]Yaoguo Y,Zhong C,Lei K,et al.Treatment of complex aortic aneurysms with fenestrated endografts and chimney stent repair:Systematic review and meta-analysis[J].Vascular,2017,25(1):92-100.doi:10.1177/1708538115627718.
[8]陆清声,景在平.腹主动脉瘤腔内治疗适应证选择及复杂病变处理[J].中华医学杂志,2016,96(45):3630-3633.doi:10.3760/cma.j.issn.0376-2491.2016.45.004.Lu QS,Jing ZP.Selection ofindications and management of complex lesions in endovascular treatment of abdominal aortic aneurysm[J].National Medical Journal of China,2016,96(45):3630-3633.doi:10.3760/cma.j.issn.0376-2491.2016.45.004.
[9]Spear R,Sobocinski J,Settembre N,et al.Early Experience of Endovascular Repair of Post-dissection Aneurysms Involving the Thoraco-abdominal Aorta and the Arch[J].Eur J Vasc Endovasc Surg,2016,5l(4):488-497.doi:10.1016/j.ejvs.2015.10.012.
[10]Cochennec F,Kobeiter H,Gohel M,et al.Early Results of Physician Modified Fenestrated Stent Grafts for the Treatment of Thoraco-abdominal Aortic Aneurysms[J].Eur J Vasc Endovasc Surg,2015,50(5):583-592.doi:10.1016/j.ejvs.2015.07.002.
[11]Liu L,Wang W,Lu QS,et al.Morphology of the ascending aorta:a study on 114 Chinese patients[J].J Intervent Med,2018,1(1):22-27.doi:10.19779/j.cnki.2096-3602.2018.01.006.
[12]Wang T,Shu C,Li M,et al.Thoracic Endovascular Aortic Repair With Single/Double Chimney Technique for Aortic Arch Pathologies[J].J Endovasc Ther,2017,24(3):383-393.doi:10.1177/1526602817698702.
[13]Wang T,Shu C,Li QM,et al.First experience with the double chimney technique in the treatment of aortic arch diseases[J].J Vasc Surg,2017,66(4):1018-1027.doi:10.1016/j.jvs.2017.02.035.
[14]Lu Q,Liu L,Chang G,et al.Mid-term outcomes from a multicenter study:Is TEVAR safe for ascending aortic dissection?[J].Int J Cardiol,2018,265:218-222.doi:10.1016/j.ijcard.2018.04.095.
[15]周敏,杨光敏,刘昭,等.应用预开窗支架技术治疗主动脉夹层动脉瘤[J].中华普通外科杂志,2019,34(4):332-335.doi:10.3760/cma.j.issn.1007-631X.2019.04.012.Zhou M,Yang GM,Liu Z,et al.Physician-modified fenestrated stent grafts for aortic dissection aneurysm[J].Zhong Hua Pu Tong Wai Ke Za Zhi,2019,34(4):332-335.doi:10.3760/cma.j.issn.1007-631X.2019.04.012.
[16]Jayet J,Heim F,Coggia M,et al.An Experimental Study of Laser in situ Fenestration of Current Aortic Endografts[J].Eur J Vasc Endovasc Surg,2018,56(1):68-77.doi:10.1016/j.ejvs.2018.03.016.
[17]Glorion M,Coscas R,McWilliams RG,et al.A Comprehensive Review of In Situ Fenestration of Aortic Endografts[J].Eur J Vasc Endovasc Surg,2016,52(6):787-800.doi:10.1016/j.ejvs.2016.10.001.
[18]Tsilimparis N,Debus ES,von Kodolitsch Y,et a1.Branched versus fenestrated endografts for endovascular repair of aortic arch lesions[J].J Vasc Surg,2016,64(3):592-599.doi:10.1016/j.jvs.2016.03.410.
[19]Kurimoto Y,Maruyama R,Ujihira K,et a1.Thoracic Endovascular Aortic Repair for Challenging Aortic Arch Diseases Using Fenestrated Stent Grafts from Zone 0[J].Ann Thorac Surg,2015,100(1):24-32.doi:10.1016/j.athoracsur.2015.01.071.
[20]Haulon S,Greenberg RK,Spear R,et al.Global experience with an inner branched arch endograft[J].J Thorac Cardiovasc Surg,2014,148(4):1709-1716.doi:10.1016/j.jtcvs.2014.02.072.
[21]Dossabhoy SS,Simons JP,Flahive JM,et al.Fenestrated endovascular aortic aneurysm repair using physician-modified endovascular grafts versus company-manufactured devices[J].J Vasc Surg,2018,67(6):1673-1683.doi:10.1016/j.jvs.2017.10.055.
[22]Yokoi Y,Azuma T,Yamazaki K.Advantage of a precurved fenestrated endograft for aortic arch disease:Simplified arch aneurysm treatment in Japan 2010 and 2011[J].J Thorac Cardiovasc Surg,2013,145(3 Suppl):S103-109.doi:10.1016/j.jtcvs.2012.11.058.
[23]范海伦,朱杰昌,戴向晨,等.台上预开窗覆膜支架置于Z1和Z0区的全腔内技术治疗主动脉弓部疾病[J].中华普通外科杂志,2018,33(12):1018-1021.doi:10.3760/cma.j.issn.1007-631X.2018.12.010.Fan HL,Zhu JC,Dai XC,et al.On table fenestrated stent graft in zone 0 and zone 1 for aortic arch diseases[J].Zhong Hua Pu Tong Wai Ke Za Zhi,2018,33(12):1018-1021.doi:10.3760/cma.j.issn.1007-631X.2018.12.010.
[24]Al-Hakim R,Schenning R.Advanced Techniques in Thoracic Endovascular Aortic Repair:Chimneys/Periscopes,Fenestrated Endografts,and Branched Devices[J].Tech Vasc Interv Radiol,2018,21(3):146-155.doi:10.1053/j.tvir.2018.06.004.
[25]Toya N,Ohki T,Fukushima S,et al.Fenestrated endovascular repair of aortic arch aneurysm in patients with bovine arch using the Najuta stent graft[J].J Vasc Surg Cases Innov Tech,2018,4(2):148-151.doi:10.1016/j.jvscit.2018.01.011.
[26]Lala S,Knowles M,Timaran D,et al.Superior mesenteric artery outcomes after fenestrated endovascular aortic aneurysm repair[J].J Vasc Surg,2016,64(3):692-697.doi:10.1016/j.jvs.2016.02.031.
