胆囊结石伴胆总管结石是肝胆外科常见病、多发病,随胆道外科微创技术的不断发展,使胆总管结石的治疗目前已趋于多样化[1]。内镜下乳头括约肌切开取石会损伤Oddi括约肌的功能,引起反流性胆管炎,且技术要求高,医疗费用大,长期饱受争议[2],此术式更适合一般情况较差、无法耐受外科手术者。目前腹腔镜下胆囊切除术并胆道探查术后一期缝合因其创伤小、恢复快、避免T管留置给患者带来身心创伤而得到广大外科医生和患者的认可,但仍存在胆汁漏、胆道感染、术中术后出血等并发症,如何降低此类并发症的发生?现对我院胆道探查术后一期缝合术前行超声引导经皮经肝穿刺胆道引流术(percutaneous transhepatic cholangial drainage,PTCD)治疗,且术后继续PTCD引流的效果进行分析,讨论PTCD在腹腔镜下胆道探查术后一期缝合中的价值。
1 资料与方法
1.1 临床资料
回顾性分析65例胆囊结石伴胆总管结石行腹腔镜下胆囊切除术并胆总管探查术患者的临床资料。男24例,女41例;年龄26~72岁;合并高血压11例,糖尿病5例,肺心病1例。向患者阐述两种术式的利弊,医学伦理学同意书上签字,根据手术方式分为PTCD组与非PTCD组,其中PTCD组33例,腹腔镜下胆道探查一期缝合并术前PTCD治疗,术后保留PTCD引流;非PTCD组32例,行腹腔镜下胆道探查术后一期缝合。对比分析两组患者一般资料比较,无统计学差异(均P>0.05),有可比性(表1)。
表1 两组一般资料比较
Table 1 Comparison of the general data between the two groups of patients
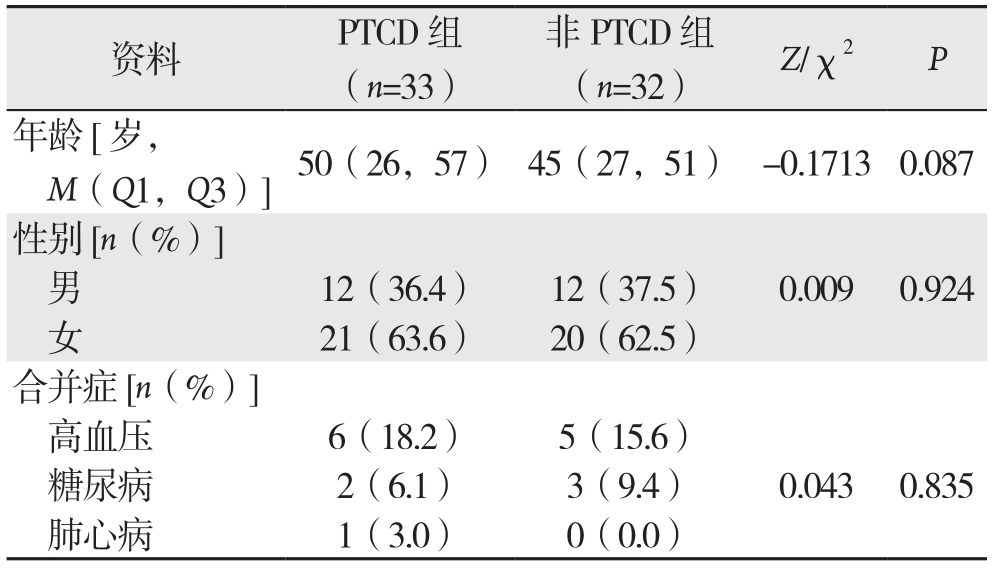
资料 PTCD组(n=33)非PTCD组(n=32) Z/χ2 P年龄[岁,M(Q1,Q3)]50(26,57) 45(27,51) -0.17130.087性别[n(%)]男12(36.4) 12(37.5) 0.009 0.924女21(63.6) 20(62.5)合并症[n(%)]高血压 6(18.2) 5(15.6)糖尿病 2(6.1) 3(9.4) 0.043 0.835肺心病 1(3.0) 0(0.0)
1.2 病例纳入标准
术前行B超及MRCP检查明确诊断为胆囊结石伴胆总管结石;胆总管直径≥1.0 cm;无严重合并症,能耐受腹腔镜手术治疗;排除肝内胆管结石;排除胆囊及胆管恶性肿瘤。
1.3 方法
1.3.1 术前准备 两组均积极完善术前相关检查,若患者年龄较大,平时心肺功能较差者予以完善心超、血气分析、肺功能检查,必要时行动态血压及动态心电图检查,并请相关科室会诊,排除不能耐受腹腔镜下手术的患者。PTCD组入院后及时B超定位下行PTCD治疗,术后保留PTCD引流。
1.3.2 手术方法 采取气管插管全麻,四孔法腹腔镜下胆囊切除术并胆道探查术,术后一期缝合,PTCD组与非PTCD组手术方法一致。分离胆囊动脉、可吸收生物夹结扎胆囊动脉并离断,分离胆囊管、可吸收生物夹夹闭胆囊管近端,胆囊管远端可用4号线或钛夹或生物夹或Hemolok结扎并用剪刀离断胆囊管,切除胆囊;解剖胆总管并用头皮针穿刺以确定是否胆总管(图1A);用手术刀切开胆总管(图1B);用胆道镜探查胆总管(图1C);取石网篮联合分离钳取出结石(图1D);取石后反复探查胆管结石是否取净并反复冲洗胆管,确定无结石残留后用4-0或5-0可吸收线间断缝合(图1E);文氏孔放置引流管,手术结束。
1.3.3 术后处理 PTCD组:术后经PTCD减压引流胆汁3~5 d,然后关闭PTCD引流管,若无腹痛腹胀,予以PTCD造影,进一步查看有无结石残留,胆道通畅情况(图1F),若无结石残留予以拔腹腔引流管及PTCD管出院,若出现结石残留,予以内镜下经十二指肠乳头切开取石、ENBD引流,复查无结石残留后拔腹腔引流管、ENBD及PTCD管出院。非PTCD组:术后6 d予以MRCP检查,确定有无结石残留,若发现结石残留,亦行内镜下经十二指肠乳头切开取石、ENBD引流,复查无结石残留后拔腹腔引流管及ENBD管出院。

图1 手术相关图片 A:穿刺确定胆管;B:尖刀切开胆管;C:胆道镜探查;D:直接或取石网篮取石;E:缝合胆管;F:经PTCD管X线造影
Figure 1 Procedure-related images A: Determination of the puncture location for the common bile duct; B: Incision of the bile duct C:Incision of the common bile duct with a sharp knife; D: Removing the stones directly or using a extraction basket; E: Closure of the common bile duct; F: Radiography through the PTCD tube
1.4 统计学处理
统计手术时间、术中出血量、术前术后直接胆红素、术后通气时间、住院时间、术后并发症、费用。利用SPSS 21.0软件分析数据,定性资料采用χ2检验,定量资料采用t检验或秩和检验。
2 结 果
2.1 两组手术情况及手术相关指标
两组所有患者均手术成功,无中转开腹病例。与非PTCD组比较,PTCD组手术时间[(119.5±24.8)min vs.(136.6±21.6)min]出血量[(44.70±16.25)mL vs.(62.81±30.69)mL],术后排气时间[(9.52±2.54)h vs. (11.13±2.31)h]均明显减少,差异均有统计学意义(均P<0.05);两组术后直接胆红素术水平均较术前下降,但两组间手术前、后直接胆红素术水平无统计学差异(均P>0.05)(表2)。
表2 两组患者手术相关指标比较( ±s)
±s)
Table 2 Comparison of the relevant surgical variables between two groups of patients ( ±s)
±s)
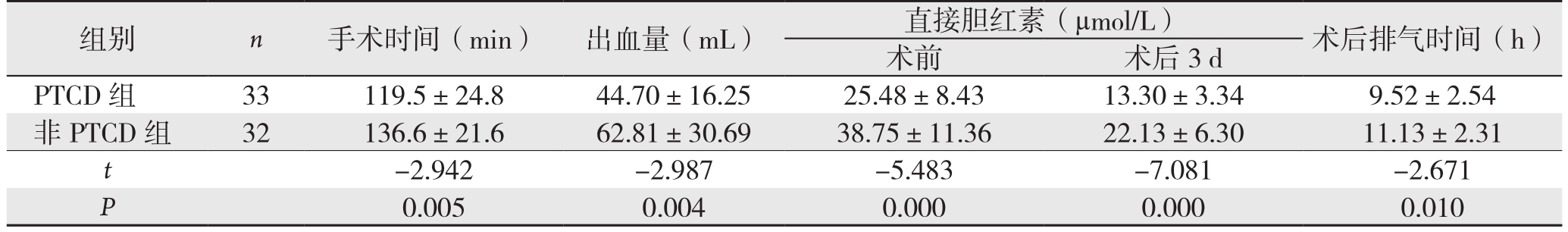
组别 n 手术时间(min) 出血量(mL) 直接胆红素(µmol/L) 术后排气时间(h)术前 术后3 d PTCD 组 33 119.5±24.8 44.70±16.25 25.48±8.43 13.30±3.34 9.52±2.54非 PTCD 组 32 136.6±21.6 62.81±30.69 38.75±11.36 22.13±6.30 11.13±2.31 t-2.942 -2.987 -5.483 -7.081 -2.671 P 0.005 0.004 0.000 0.000 0.010
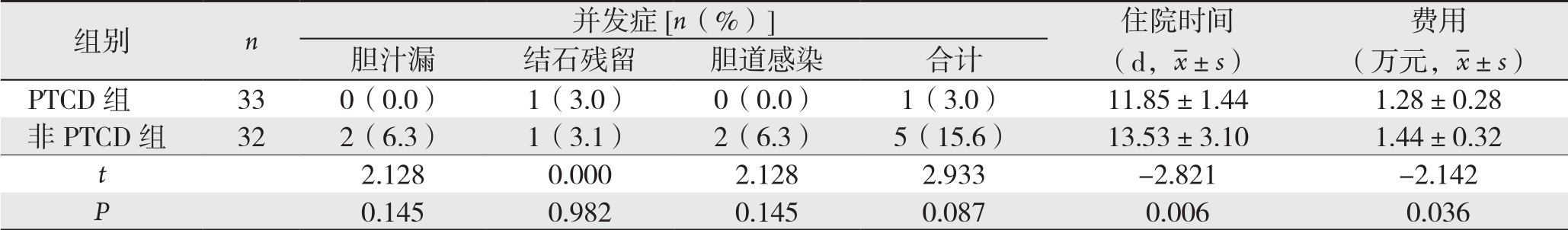
2.2 两组并发症情况与术后住院时间、费用
PTCD组出现1例PTCD穿刺后胆道出血,量少,予以通畅引流后自行停止,2例PTCD穿刺后引流管阻塞,予以冲洗或调整引流位置后引流通畅。两组术后均出现1例结石残留,通过内镜下经十二指肠乳头切开取石、鼻胆管引流,术后痊愈出院;非PTCD组出现2例胆汁漏,引流管通畅引流,以及持续冲洗负压吸引等保守治疗痊愈;非PTCD组出现2例胆道感染,通过术后抗生素等保守治疗痊愈。两组术后并发症(结石残留、胆汁漏、胆道感染)单项与总并发症发生率比较,差异均无统计学意义(均P>0.05);PTCD组的住院时间及费用均少于非PTCD组(均P<0.05)(表3)。
表3 两组术后并发症与住院时间及费用比较
Table 3 Comparison of the postoperative complications as well as length of hospital stay and costs between the two groups

3 讨 论
目前腹腔镜下胆囊切除术并胆总管探查术因其微创及较低的并发症发生率逐步得到广泛的应用和认可[3-5],然而随腹腔镜技术的日益发展,胆道探查术式较多,主要有腹腔镜下经胆囊管胆总管探查术、经胆总管切开胆总管探查术+T管引流术、经胆总管切开胆道探查术后一期缝合等术式。经胆囊管胆总管探查术,胆道镜需从胆囊管进入胆总管,对术者腔镜技术要求很高,且胆囊管内径需相对较扩张,适应证较小且难度很高;腹腔镜下胆总管探查+T管引流术为主要治疗手术[6],然而切开胆总管后放置的T管可能会出现胆汁漏、T管脱落、胆汁性腹膜炎等并发症[7],还会带来诸多问题,如术后电解质、消化液、消化酶的大量流失,长期带管出院可能引起胆道感染,患者生活质量下降,治疗时间延长,医疗费用增加等[8-9]。经胆总管切开胆道探查术并一期缝合因创伤小,恢复快,逐步得到外科医生及患者的接受,Khaled等[10]研究指出,对于胆管无明显炎症、狭窄、术中胆管探查显示胆管远端通畅、结石取尽者,不应常规放置T管。然而一期缝合后缺少T管对胆道的减压引流,可能存在胆汁漏、胆汁性腹膜炎、胆道感染等并发症,故研究胆道探查术并一期缝合术后胆道减压引流的方式十分有必要。
本研究通过胆道探查术并一期缝合术前行PTCD治疗、术后保留PTCD引流,与胆道探查术后一期缝合术行对比分析,研究PTCD在胆道探查术后一期缝合中的价值。结果显示,手术时间、术中出血量、术前直接胆红素、术后3 d直接胆红素、术后通气时间、住院时间、费用等各项,PTCD组明显优于非PTCD组。现讨论其原因如下:⑴ 术前PTCD引流,可以有效胆汁引流,降低胆红素水平,恢复肝功能,降低术前住院天数;⑵ 术前PTCD引流,可以明显胆道减压、减少胆道的炎症,胆道充血水肿轻,有利于手术操作,降低手术时间及出血量;⑶ PTCD组因手术时间短、炎症轻、出血量少,术后通气早,进食早,恢复更快;⑷ 术后继续PTCD引流,进一步引流胆汁,降低胆红素,恢复肝功能,降低平均住院日;⑸ 术后继续PTCD引流,有效引流胆汁,降低胆道压力,有利于预防术后胆道感染、胆汁漏;⑹ 术后经PTCD管造影检查结石残留情况,费用更低。本资料中非PTCD组中发生2例胆瘘、2例胆道感染,PTCD组中无胆瘘、胆道感染发生,虽然最后数据无统计学意义,但术后PTCD引流的情况下,胆道压力可以得到有效的减低,降低胆道感染可能,有利于胆管壁愈合,有利于预防术后胆汁漏。
胆汁漏是胆总管探查术后一期缝合中最常见的并发症[11-14],原因可能有:⑴ 胆道炎症较重,管壁充血水肿,缝合效果较差;⑵ 一期缝合时,反复加针,针距较密,打结用力过大,造成胆管切割;⑶ 选择缝针及线较粗,导致从针眼处渗漏。一期缝合术后胆汁漏一般发生率为10%以上[1,6],而我院一期缝合术后胆汁漏发生率为3.1%(2/65),发生率低,原因可能有:⑴ 腹腔镜手术的广泛开展,腹腔镜器械的不断更新及腹腔镜下缝合技术的日益提高;⑵ 胆管壁采用手术刀直接切开,避免电刀致胆管壁发生凝固性坏死,降低胆管壁愈合难度[15];⑶ 选择4-0或5-0可吸收线缝合,降低了缝针及线较粗致针眼处渗漏;⑷ TCD组中未出现胆汁漏,术前PTCD引流,有效胆汁引流及胆道减压,胆道炎症轻,管壁充血水肿轻;术后PTCD继续引流,有效胆汁引流及胆道减压,降低了胆汁漏及胆道感染的风险。
PTCD是一种微创的肝内胆管置管引流术[16],特点是可以快速解除梗阻,达到减轻黄疸的目的,具有简捷方便、患者损伤及痛苦小、感染率低等优点[17]。经多年临床应用开展,PTCD技术目前已十分成熟,成功率已接近100%[17-18]。穿刺技术要点:⑴ 精确彩超定位,辨清胆管与血管,避免出血;⑵ 利用彩超实时监视的优势,选择直径0.4 cm以上的胆管[19];⑶ 穿刺针与目标胆管平行或成顿角,能更好的穿刺与导丝置入;⑷ 避免暴力穿刺,是避免胆道出血的关键[20]。主要并发症[21]:胆道出血、胆道感染、引流管移位、脱出、阻塞。胆道出血是PTCD常见并发症,临床医生应引起重视[22],在穿刺过程中,应尽量避免暴力穿刺而引起出血和术后感染;引流管阻塞时,可反复冲洗至通畅;引流管移位时可在X线下进行胆管造影[23],调整引流管位置。多数并发症为轻型并发症,对症治疗后好转[24],本资料中PTCD组出现1例PTCD穿刺后胆道出血,量少,予以通畅引流后自行停止,2例PTCD穿刺后引流管阻塞,予以冲洗或调整引流位置后引流通畅。超声定位下经皮经肝穿刺胆道引流术能促进患者康复,减少并发症,能更好地被患者接受[24]。
腹腔镜下胆道探查术后一期缝合行术前PTCD治疗,可通畅引流胆汁,降低胆红素,恢复肝功能,胆道减压、降低炎症,有利于手术操作,手术时间短,出血量少。术后继续PTCD引流,可以继续降低胆红素,恢复肝功能,减低胆管压力、炎症,有利于胆管壁愈合,降低胆汁漏、胆道感染。患者恢复快,平均住院日及费用低。胆道探查术后一期缝合时,即使没有严重肝功能损伤,术前经超声检查胆总管直径≥1.0cm,亦可置入PTCD引流,有利于术前术后肝功能恢复、降低平均住院日及费用,值得临床推广。
参考文献
[1] 尹飞飞, 李学民, 段希斌, 等. 不留置T管引流治疗胆囊结石并胆总管结石的临床疗效[J]. 中国普通外科杂志, 2016, 25(8):1112–1116. doi:10.3978/j.issn.1005–6947.2016.08.004.Yin FF, Li XM, Duan XB, et al. Clinical efficacy of T-tube-free approach in treatment of gallbladder stones and concomitant common bile duct stones[J]. Chinese Journal of General Surgery,2016, 25(8):1112–1116. doi:10.3978/j.issn.1005–6947.2016.08.004.
[2] Costi R, Gnocchi A, Di Mario F, et al. Diagnosis and management of choledocholithiasis in the golden age of imaging, endoscopy and laparoscopy[J]. World J Gastroenterol, 2014, 20(37):13382–13401.doi: 10.3748/wjg.v20.i37.13382.
[3] Lu J, Xiong XZ, Cheng Y, et al. One-stage versus two-stage management for concomitant gallbladder stones and common bile duct stones in patients with obstructive jaundice[J]. Am Surg, 2013,79(11):1142–1148.
[4] Lee HM, Min SK, Lee HK. Long-term results of laparoscopic common bile duct exploration by choledochotomy for holedocholithiasis: 15-year experience from a single center[J]. Ann Surg Treat Res, 2014, 86(1):1–6. doi: 10.4174/astr.2014.86.1.1.
[5] Savita KS, Bhartia VK. Laparoscopic CBD Exploration[J]. Indian J Surg, 2010, 75(5):395–399. doi: 10.1007/s12262–010-0157–6.
[6] 张淼, 谈永飞. 腹腔镜下经胆囊管胆总管探查术与胆总管探查并一期缝合术治疗胆总管结石的对比研究[J]. 中国普通外科杂志,2017, 26(2):151–156. doi:10.3978/j.issn.1005–6947.2017.02.004.Zhang M, Tan YF. Comparison of laparoscopic transcystic common bile duct exploration and laparoscopic common bile duct exploration with primary suture for common bile duct stones[J].Chinese Journal of General Surgery, 2017, 26(2):151–156.doi:10.3978/j.issn.1005–6947.2017.02.004.
[7] 潘步建, 徐迈宇, 陈峰, 等. 腹腔镜下经胆囊管纤维胆道镜取石术治疗胆总管结石的临床研究[J]. 中华普通外科杂志, 2015,30(6):485–486. doi:10.3760/cma.j.issn.1007–631X.2015.06.018.Pan BJ, Xu MY, Chen F, et al. Clinical study on laparoscopic stone extraction through fiber choledochoscope for choledocholithiasis[J].Zhong Hua Pu Tong Wai Ke Za Zhi, 2015, 30(6):485–486.doi:10.3760/cma.j.issn.1007–631X.2015.06.018.
[8] Wu X, Yang Y, Dong P, et al. Primary closure versus T-tube drainage in laparoscopic common bile duct exploration: a meta analysis of randomized clinical trials[J]. Langenbecks Arch Surg,2012, 397(6):909–916. doi: 10.1007/s00423–012-0962–4.
[9] 田雨, 吴硕东. 肝内外胆管结石微创治疗方法和技术的改进[J]. 临床肝胆病杂志, 2017, 33(2):253–255. doi:10.3969/j.issn.1001–5256.2017.02.008.Tian Y, Wu SD. Improvement of minimally invasive therapies and techniques for intra-and extrahepatic bile duct stones[J].Journal of Clinical Hepatology, 2017, 33(2):253–255. doi:10.3969/j.issn.1001–5256.2017.02.008.
[10] Khaled YS, Malde DJ, de Souza C, et al. Laparoscopic bile duct exploration via choledochotomy followed by primary duct closure is feasible and safe for the treatment of choledocholithiasis[J]. Surg Endosc, 2013, 27(11):4164–4170. doi: 10.1007/s00464–013-3015–3.
[11] Tan KK, Shelat VG, Liau KH, et al. Laparoscopic common bile duct exploration:our first 50 cases[J]. Ann Acad Med Singapore,2010, 39(2):136–142.
[12] Zhu QD, Tao CL, Zhou MT, et al. Primary closure versus T-tube drainage after common bile duct exploration for choledocholithiasis[J].Langenbecks Arch Surg, 2011, 396(1):53–62. doi: 10.1007/s00423–010-0660-z.
[13] Pawa N, Tutton MG. Primary common bile duct closure is safe following emergency and elective exploration [J]. World J Surg,2009, 33(8):1779. doi: 10.1007/s00268–009-0028–0.
[14] 徐键. 腹腔镜下经胆囊管胆总管探查取石术的临床应用体会[J]. 中国现代医药杂志, 2015, 17(10):41–44. doi:10.3969/j.issn.1672–9463.2015.10.010.Xu J. The clinical application and experience of laparoscopic transcystic common bile duct exploration[J]. Modern Medicine Journal of China, 2015, 17(10):41–44. doi:10.3969/j.issn.1672–9463.2015.10.010.
[15] 潘峥, 程张军, 刘胜利, 等. 胆总管结石腹腔镜胆总管探查术后一期缝合与T管引流的临床比较[J]. 中国普通外科杂志, 2015,24(8):1135–1139. doi:10.3978/j.issn.1005–6947.2015.08.016.Pan Z, Cheng ZJ, Liu SL, et al. Primary closure versus T-tube drainage following laparoscopic common bile duct exploration for choledocholithiasis[J]. Chinese Journal of General Surgery, 2015,24(8):1135–1139. doi:10.3978/j.issn.1005–6947.2015.08.016.
[16] 周亚龙, 程千里, 林云志, 等. PTCD 治疗合并感染性休克的急性梗阻性化脓性胆管炎的疗效及安全性分析[J]. 湖南师范大学学报:医学版, 2015, 12(3):140–141.Zhou YL, Cheng QL, Lin YZ, et al. Analysis of the effects and safety of PTCD for acute obstructive suppurative cholangitis combined with infectious shock[J]. Journal of Hunan Normal University: Medical Science, 2015, 12(3):140–141.
[17] 刘国华, 狄长安, 梁峰, 等. 超声引导下经皮经肝穿刺胆管引流术治疗梗阻性黄疸的临床应用价值[J]. 中国医刊, 2016, 51(5):103–104. doi:10.3969/j.issn.1008–1070.2016.05.033.Liu GH, Di CA, Liang F, et al. Application value of percutaneous transhepatic cholangial drainage under ultrasound guidance in treatment of obstructive jaundice[J]. Chinese Journal of Medicine,2016, 51(5):103–104. doi:10.3969/j.issn.1008–1070.2016.05.033.
[18] 敖劲, 曾令雯, 蔡争, 等. 急性梗阻性化脓性胆管炎经皮肝穿刺胆道引流术后死亡原因分析[J]. 中国普通外科杂志, 2015,24(8):1195–1197. doi:10.3978/j.issn.1005–6947.2015.08.028.Ao J, Zeng LW, Cai Z, et al. Clinical analysis of causes of death after percutaneous transhepatic choledochal drainage for acute obstructive suppurative cholangitis[J]. Chinese Journal of General Surgery, 2015, 24(8):1195–1197. doi:10.3978/j.issn.1005–6947.2015.08.028.
[19] 许爱国, 郭晓东, 华军霞. 28例胆囊切除术致胆管损伤的临床分析[J]. 中国医学前沿杂志:电子版, 2014, 6(6):138–140.Xu AG, Guo XD, Hua JX. 28 case clinic analyse iatrogenic bile duct injury in laparoscopic cholecystectomy and miniincision open cholecystectomy[J]. Chinese Journal of the Frontiers of Medical Science: Electronic Version, 2014, 6(6):138–140.
[20] Tsuyuguchi T, Miyakawa K, Sugiyama H, et al. Ten-year long-term results after non-surgical management of hepatolithiasis, including cases with choledochoenterostomy[J]. J Hepatobiliary Pancreat Sci,2014, 21(11):795–800. doi: 10.1002/jhbp.134.
[21] 符真, 张剑权, 周帅. 胆道镜经皮肝穿刺胆道造瘘取石治疗肝内胆管结石42例临床分析[J]. 中国现代医学杂志, 2017,27(13):127–128. doi:10.3969/j.issn.1005–8982.2017.13.028.Fu Z, Zhang JQ, Zhou S. Clinical analysis of percutaneous transhepatic choledochoscopic stone extraction for intrahepatic stones in 42 cases[J]. China Journal of Modern Medicine, 2017,27(13):127–128. doi:10.3969/j.issn.1005–8982.2017.13.028.
[22] Lim JU, Joo KR, Cha JM, et al. Needle-knife fistulotomy with percutaneous transhepatic cholangioscopy for managing complete bilioenteric anastomosis occlusion[J]. Surg Laparosc Endosc Percutan Tech, 2014, 24(1):e10–2. doi: 10.1097/SLE.0b013e31828e4000.
[23] 牛乐军, 金颖, 刘大千, 等. 超声引导下经皮经肝穿刺胆管造影与置管引流32例分析[J]. 人民军医, 2016, 59(1):70–71.Niu LJ, Jin Y, Liu DQ, et al. Analysis of ultrasound-guided percutaneous transhepatic cholangiography and drainage in 32 cases[J]. People's Military Surgeon, 2016, 59(1):70–71.
[24] Ma S, Hu S, Gao F, et al. Endoscopy lithotomy for intrahepatic gallstones: a meta-analysis[J]. Surg Laparosc Endosc Percutan Tech, 2015, 25(4):269–274. doi: 10.1097/SLE.0000000000000138.
