甲状腺癌是内分泌系统常见恶性肿瘤,近20年其在全球范围内发病率呈逐渐上升趋势,且尤以甲状腺微小乳头状癌(PTMC)更为显著[1]。PTMC临床表现差异较大,目前国内外尚无明确的诊疗规范[2]。本研究回顾性分析2011年6月—2016年5月我科收治的PTMC病例,并基于国内外指南及文献报道,对PTMC诊治经验进行总结并提出意见供同行评议。
1 资料与方法
1.1 一般资料
2011年6 月—2016年5月,中日友好医院普外科三部手术治疗PTMC患者47例,其中男9例,女38例;年龄27~78岁,平均(46.3±12.1)岁,其中<45岁22例;病程3 d至8年,平均(12.4±23.7)个月。
1.2 术前辅助检查
47例均行术前超声检查(表1),超声表现为低回声结节43例(91.5%),形态欠规则17例(36.2%),边界欠清23例(48.9%),沙砾样钙化33例(70.2%),多发结节23例(48.9%),中央区(6组)淋巴结肿大6例(12.8%),颈侧方(2、3、4组)淋巴结肿大10例(21.3%)。其中14例行超声引导下细针穿刺细胞学检查(FNA),11例(78.6%)穿刺病理明确诊断为甲状腺乳头状癌,余3例穿刺仅提示细胞异型性。
表1 PTMC术前超声特征
Table 1 Ultrasound features of PTMC
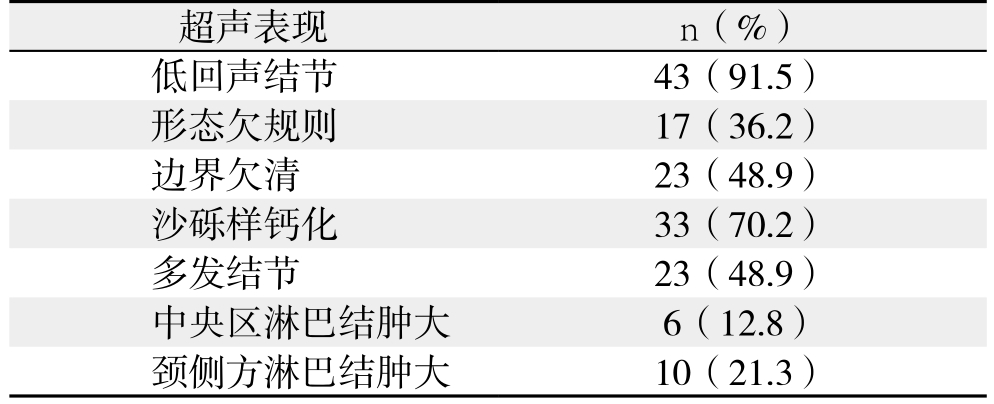
超声表现 n(%)低回声结节 43(91.5)形态欠规则 17(36.2)边界欠清 23(48.9)沙砾样钙化 33(70.2)多发结节 23(48.9)中央区淋巴结肿大 6(12.8)颈侧方淋巴结肿大 10(21.3)
1.3 治疗方法
47例患者均行手术治疗,根据患者性别、年龄、肿瘤病灶情况、术中淋巴结探查及冷冻病理结果确定手术方案,颈部淋巴结清扫范围依照2012年《甲状腺结节和分化型甲状腺癌诊治指南》[3]。
1.4 术后治疗及随访
患者术后均予左旋甲状腺素片口服治疗,并参考2012年10月我国《甲状腺结节及分化型甲状腺癌指南》,基于双风险评估结果进行术后个体化TSH抑制治疗[3]。对于病理证实有淋巴结转移或为高危人群(已行全或近全甲状腺切除术)患者,建议行放射性I131治疗。术后随访3~62个月,无复发、转移及死亡病例。
1.5 统计学处理
采用SAS 9.2进行数据分析,正态性分布的连续性数值变量采用t检验或单因素方差分析进行统计检验,非正态性数据采用Wilcoxon检验或Kruskal-Wallis检验。计数资料采用χ2检验进行统计分析。P<0.05为差异有统计学意义。
2 结 果
2.1 手术方式与术后病理结果
47例均经石蜡病理证实为PTMC,根据第6版UICC分化型甲状腺癌分期标准进行分期:I期39例,III期5例,IV期3例;病灶长径(0.68±0.23)cm;21例(44.7%)为多发病灶(2~5枚,平均病灶数目2.7枚),其中14例(29.8%)为双侧甲状腺多发病灶(2~5枚,平均病灶数目3.4枚)。淋巴结转移情况:29例患者行颈淋巴结清扫术,14例发生转移,男女比例1:6,>45岁8例,其中中央区淋巴结转移率48.3%(14/29)。15例患者行颈侧区淋巴结清扫,颈侧区淋巴结转移率53.3%(8/15),且该8例患者中央组淋巴结均为阳性,无跳跃转移病例。手术方式及病灶数目、淋巴结转移情况见表2。
表2 47例PTMC患者手术方式及病灶数目、淋巴结转移情况
Table 2 Surgical procedures, lesion number and lymph node metastasis of the 47 PTMC patients

注:Ia期为中央区淋巴结转移;Ib期为单侧、双侧颈侧区、或纵膈淋巴结转移
Note: Ia stage representing central lymph node metastasis; Ib stage representing unilateral or bilateral lymph node metastasis or mediastinal lymph node metastasis
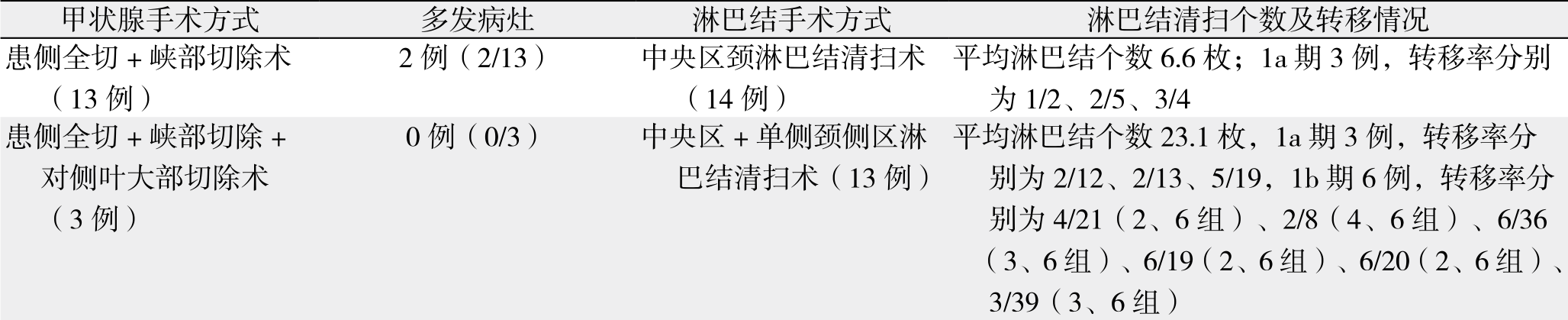 双侧甲状腺全切术(31例)平均淋巴结个数39枚;均为Ib期,转移率分别为2/38(4、6组)、21/40(4、6组)19例(19/31,单侧病灶5例,双侧病灶14例)中央区+双侧颈侧区淋巴结清扫术(2例)
双侧甲状腺全切术(31例)平均淋巴结个数39枚;均为Ib期,转移率分别为2/38(4、6组)、21/40(4、6组)19例(19/31,单侧病灶5例,双侧病灶14例)中央区+双侧颈侧区淋巴结清扫术(2例)
2.2 临床病理因素与淋巴结转移的关系
对行淋巴结清扫的29例患者临床病理因素进行统计分析,发现仅肿瘤是否侵犯包膜与淋巴结转移的发生有关(P=0.035),而与年龄、肿瘤大小、是否多发病灶、是否双侧病灶均与淋巴结转移无关(均P>0.05)(表3)。
2.3 术后并发症
共有8例患者术后发生并发症,其中5例为术后暂时性甲状旁腺功能不全,表现为术后1~2 d出现手足麻木甚至四肢短暂抽搐现象,查血清钙(1.73±0.24)mmol/L,予以静脉应用10%葡萄糖酸钙20~30 mL/d后症状好转,之后予以门诊口服补充钙剂及维生素D制剂并逐渐减量,无需长期补钙病例。切口积液1例,经引流换药愈合。暂时性喉返神经损伤1例,声音嘶哑6个月后自行恢复,复查喉镜声带运动恢复正常。暂时性喉上神经损伤1例,出现饮水呛咳,症状2周后自行缓解。
表3 29例淋巴结清扫患者临床病理因素与淋巴结转移的关系
Table 3 Relationship between clinicopathologic factors and lymph node metastasis of the 29 patients undergoing lymph node dissection
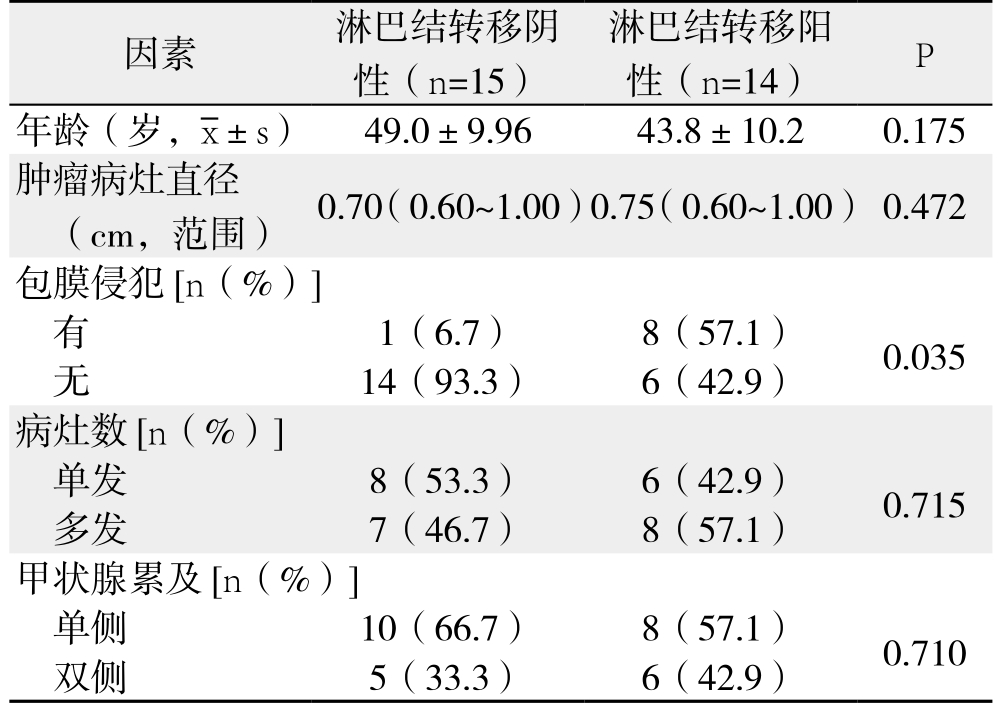
因素 淋巴结转移阴性(n=15)淋巴结转移阳性(n=14) P年龄(岁, ±s) 49.0±9.96 43.8±10.2 0.175肿瘤病灶直径(cm,范围) 0.70(0.60~1.00)0.75(0.60~1.00) 0.472包膜侵犯[n(%)]有1(6.7) 8(57.1) 0.035无14(93.3) 6(42.9)病灶数[n(%)]单发 8(53.3) 6(42.9) 0.715多发 7(46.7) 8(57.1)甲状腺累及[n(%)]单侧 10(66.7) 8(57.1) 0.710双侧 5(33.3) 6(42.9)
±s) 49.0±9.96 43.8±10.2 0.175肿瘤病灶直径(cm,范围) 0.70(0.60~1.00)0.75(0.60~1.00) 0.472包膜侵犯[n(%)]有1(6.7) 8(57.1) 0.035无14(93.3) 6(42.9)病灶数[n(%)]单发 8(53.3) 6(42.9) 0.715多发 7(46.7) 8(57.1)甲状腺累及[n(%)]单侧 10(66.7) 8(57.1) 0.710双侧 5(33.3) 6(42.9)
3 讨 论
近年来,甲状腺癌发病率迅速增长[4-5],特别是PTMC,不同报道中PTMC占甲状腺癌发病的6%~35%不等[6]。PTMC以青壮年多发,且女性多见,本组病例中发病平均年龄为46.3岁,男女比例1:4,PTMC生长缓慢,一般无特殊临床表现,本组患者中44例(93.6%)为体检发现甲状腺肿物。
在诊断方面,国内有将术前行甲状腺穿刺细胞学检查指征扩大的趋势,尽管细针穿刺细胞学检查(FNA)对甲状腺结节的诊断准确性较高,但受目标结节大小、位置及穿刺者技术、病理切片制作等因素影响,有2%~20%的甲状腺穿刺细胞学标本不能给出明确诊断,而没有明确诊断的FNA仍然有1.7%~6.6%的恶性风险[7-8]。
本组共14例患者(29.8%)行FNA,其中11例(78.6%)穿刺病理明确诊断为甲状腺乳头状癌,余3例穿刺仅提示细胞异型性。从诊断经验上笔者认为术前超声具有2项以上甲状腺彩色多普勒恶性结节特征者,或伴有甲状腺癌高危因素、查体甲状腺内包块质硬固定、伴有声音嘶哑等肿瘤侵犯症状者,不推荐对甲状腺结节常规行穿刺活检术,可考虑直接行手术治疗。常规超声诊断不明确者,对直径>5 mm的PTMC可进行FNA,建议在超声引导下行细针穿刺活检,应用Bethesda诊断系统进行分类[8]。
微小癌的治疗在甲状腺癌治疗中争议较大,国内外指南建议对于无淋巴结转移及周围组织浸润、非病理学高危亚型等的低危甲状腺微小癌患者,可采用密切随访观察,待出现肿瘤直径增大、淋巴结转移、周围组织浸润等新的危险因素时再采取手术干预[2,9]。但甲状腺微小癌从生物学行为考虑其依然为恶性肿瘤,部分生物学行为较差,易发生区域淋巴结转移,多数学者认为应积极手术治疗[10-11]。
文献[12-14]报道甲状腺微小癌中多发病灶发生率为18%~87%,多发病灶及双侧病灶者概率也较高,其与淋巴结转移、远处转移及术后复发均有直接关系,预示了多发灶微小甲状腺癌侵袭性的生物学特点。本组47例PTMC病例中,23例(48.9%)术前超声提示为多发性结节,术后病理证实21例(44.7%)为多发肿瘤病灶,其中14例(29.8%)为双侧甲状腺多发病灶,主病灶以外多发病灶大小仅为0.01~0.70 cm。笔者认为PTMC患者中确有早期出现多发病灶、颈部淋巴结转移甚至远处转移的病例。对术前超声已提示多发病灶、术中探查可疑多发结节或存在高危因素患者(淋巴结或远处转移、甲状腺包膜侵犯、细胞学高度恶性、迅速进展、肿瘤紧邻气管或喉返神经),双侧甲状腺全切应为首选治疗方式。
目前对于低危甲状腺癌患者是否进行预防性中央区淋巴结清扫存在较大争议,尤其微小癌患者。美国Seer数据库1998—2010年共计29 512例手术治疗的甲状腺癌患者,其中73.4%行双侧甲状腺全切,38.4%行中央区±颈侧区淋巴结清扫,淋巴结阳性率达30.3%[12]。国内外多篇文献[15-18]报道PTMC存在31%~64.1%的淋巴结转移率。多项研究[11,19-21]建议行预防性中央区淋巴结清扫,对于专业的甲状腺外科医生中央区淋巴结清扫并不会增加甲状旁腺和喉返神经损伤的风险[22-23]。
最终本组29例患者行颈淋巴结清扫,其中中央区淋巴结阳性率高达48.3%(14/29),男女比例为1:6,>45岁者仅8例,肿瘤侵犯包膜8例。临床病理因素统计分析发现仅肿瘤侵犯包膜与淋巴结转移的发生具有相关性。本组15例行颈侧区淋巴结清扫患者,颈侧区淋巴结转移率高达53.3%(8/15),且这8例患者中央组淋巴结均为阳性,无跳跃转移病例。如此高的淋巴结阳性率证实也了本组患者淋巴结清扫策略的合理性。笔者认为超声对中央区转移淋巴结转移诊断敏感性较低,对颈侧区淋巴结转移诊断相对敏感。故对于术前超声提示或术中探查存在中央组淋巴结肿大,或存在淋巴结转移高危因素的患者,预防性中央区淋巴结清扫结合术中冰冻病理检查是必要的,一方面可减少局部复发风险,降低复发时重要器官受侵犯的可能性,亦可规避再次手术时损伤喉返神经及甲状旁腺的风险。
而对肿瘤侵犯包膜伴中央区淋巴结阳性、以颈淋巴结转移为首发症状及发现颈侧区淋巴结肿大的患者,颈侧区淋巴结清扫术是必要的。对于低危患者,术中探查颈侧区淋巴结无肿大者,不作预防性颈侧区淋巴结清扫,当复发出现颈侧区淋巴结肿大可再次手术清扫,手术难度不大。
综上所述,对于PTMC的术前诊断,彩色多普勒超声是首选,甲状腺外科医生要熟悉甲状腺癌超声特点,不建议盲目扩大FNA的指征。对于可疑病例,建议采取积极手术治疗。对于术前超声已提示多发结节、术中探查可疑多发结节或存在高危因素者,手术建议行双侧甲状腺全切。预防性中央组淋巴结清扫结合术中冰冻病理是必要的,可以了解是否存在肉眼不能判断的淋巴结转移可能,能够确定个体化手术切除范围,为术后治疗提供基础及依据。
参考文献
[1] Malandrino P, Pellegriti G, Attard M, et al. Papillary thyroid microcarcinoma: A comparative study of the characteristics and risk factors at presentation in two cancer registries [J]. J Clin Endocrinol Metab, 2013, 98(4): 1427–1434. doi: 10.1210/jc.2012–3728.
[2] 中国抗癌协会甲状腺癌专业委员会(CATO). 甲状腺微小乳头状癌诊断与治疗中国专家共识(2016版)[J]. 中国肿瘤临床, 2016,43(10):405–411. doi:10.3969/j.issn.1000–8179.2016.10.001.Chinese Association of Thyroid Oncolog (CATO). Chinese expert consensus on diagnosis and treatment of papillary thyroid microcarcinoma (2016 edition)[J]. Chinese Journal of Clinical Oncology, 2016, 43(10):405–411. doi:10.3969/j.issn.1000–8179.2016.10.001.
[3] 中华医学会内分泌学分会, 中华医学会外科学分会内分泌学组,中国抗癌协会头颈肿瘤专业委员会, 等. 甲状腺结节和分化型甲状腺癌诊治指南[J]. 中华内分泌代谢杂志, 2012, 28(10):779–797.doi:10.3760/cma.j.issn.1000–6699.2012.10.002.Chinese Society of Endocrinology, Endocrinology Group of Chinese Society of Surgery, Committee of Head and Neck Oncology of Chinese Anti-Cancer Association, et al. Guidelines for diagnosis and treatment of thyroid nodule and differentiated thyroid carcinoma[J].Chinese Journal of Endocrinology and Metabolism, 2012,28(10):779–797. doi:10.3760/cma.j.issn.1000–6699.2012.10.002.
[4] Li N, Du XL, Reitzel LR, et al. Impact of enhanced detection on the increase in thyroid cancer incidence in the United States: review of incidence trends by socioeconomic status within the surveillance,epidemiology, and end results registry, 1980–2008[J]. Thyroid,2013, 23(1):103–110. doi: 10.1089/thy.2012.0392.
[5] 刘玉琴, 张书全, 陈万青, 等. 中国2003–2007年甲状腺癌发病死亡现状及流行趋势分析[J]. 中华流行病学杂志, 2012,33(10):1044–1048. doi:10.3760/cma.j.issn.0254–6450.2012.10.011.Liu YQ, Zhang SQ, Chen WQ, et al. Trend of incidence and mortality on thyroid cancer in China during 2003–2007[J]. Chinese Journal of Epidemiology, 2012, 33(10):1044–1048. doi:10.3760/cma.j.issn.0254–6450.2012.10.011.
[6] Yang GC, LiVolsi VA, Baloch ZW. Thyroid microcarcinoma: fine needle aspiration diagnosis and histologic follow-up[J]. Int J Surg Pathol, 2002, 10(2):133–139.
[7] Grani G, Calvanese A, Carbotta G, et al. Intrinsic factors affecting adequacy of thyroid nodule fine-needle aspiration cytology[J].Clin Endocrinol (Oxf), 2013, 78(1):141–144. doi: 10.1111/j.1365–2265.2012.04507.x.
[8] Bongiovanni M, Spitale A, Faquin WC, et a1. The Bethesda System for reporting thyroid cytapathology:a meta-analysis[J]. Acta Cytol, 2012, 56(4):333–339. doi: 10.1159/000339959.
[9] Oda H, Miyauchi A, Ito Y, et al. Incidences of Unfavorable Events in the Management of Low-Risk Papillary Microcarcinoma of the Thyroid by Active Surveillance Versus Immediate Surgery[J].Thyroid, 2016, 26(1):150–155. doi: 10.1089/thy.2015.0313.
[10] Mantinan B, Rego-Iraeta A, Larrañaga A, et al. Factors influencing the outcome of patients with incidental papillary thyroid microcarcinoma[J]. J Thyroid Res, 2012, 2012:469397. doi:10.1155/2012/469397.
[11] 吴唯, 钱立元, 陈学东, 等. 分化型甲状腺微小癌的诊断和治疗: 附138例报道[J]. 中国普通外科杂志, 2015, 24(5):627–632.doi:10.3978/j.issn.1005–6947.2015.05.002.Wu W, Qian LY, Chen XD, et al. Diagnosis and treatment of differentiated thyroid microcarcinoma: a report of 138 cases[J].Chinese Journal of General Surgery, 2015, 24(5):627–632.doi:10.3978/j.issn.1005–6947.2015.05.002.
[12] Wang TS, Goffredo P, Sosa JA, et al. Papillary thyroid microcarcinoma: an over-treated malignancy [J]? World J Surg,2014, 38(9):2297–2303. doi: 10.1007/s00268–014–2602–3.
[13] 严丽, 李清怀, 冀宏, 等. 多灶甲状腺微小乳头状癌的临床特征分析[J]. 中国普通外科杂志, 2016, 25(11):1568–1572. doi:10.3978/j.issn.1005–6947.2016.11.008.Yan L, Li QH, Ji H, et al. Clinical features of multifocal papillary thyroid microcarcinoma[J]. Chinese Journal of General Surgery, 2016, 25(11):1568–1572. doi:10.3978/j.issn.1005–6947.2016.11.008.
[14] Shattuck TM, Weatra WH,Ladenson PW, et al. Independent clonal origins of distinct tumor foci in multifocal papillary thyroid carcinoma[J]. N Engl J Med, 2005, 352(23):2406–12.
[15] Lim YC, Choi EC, Yoon YH, Kim EH, Koo BS. Central lymph node metastases in unilateral papillary thyroid microcarcinoma[J].Br J Surg, 2009, 96(3):253–257. doi: 10.1002/bjs.6484.
[16] Roh JL, Kim JM, Park CI. Central cervical nodal metastasis from papillary thyroid microcarcinoma: pattern and factors predictive of nodal metastasis [J]. Ann Surg Oncol, 2008, 15(9):2482–2486. doi:10.1245/s10434–008–0044–6.
[17] 李治, 赵群仔, 屈新才, 等. 乳头状甲状腺微小癌的颈部中央组淋巴结转移[J]. 中华普通外科杂志, 2013, 28(1):28–30. doi:10.3760/cma.j.issn.1007–631X.2013.01.010.Li Z, Zhao QZ, Qu XC, et al. Cervical lymph node metastasis of papillary thyroid microcarcinoma[J]. Zhong Hua Pu Tong Wai Ke Za Zhi, 2013, 28(1):28–30. doi:10.3760/cma.j.issn.1007–631X.2013.01.010.
[18] 王卓颖, 孙团起, 吴毅, 等. 中央区淋巴结清扫在甲状腺乳头状微小癌治疗中的意义(附10年1048例报告)[J]. 中国实用外科杂志,2014, 34(1):93–96.Wang ZY, Sun TQ, Wu Y, et al. Central lymph node dissection for non-incidental papillary thyroid microcarcinoma: 10 years’experience[J]. Chinese Journal of Practical Surgery, 2014, 34(1):93–96.
[19] 王志军, 李玉龙, 彭德峰, 等. 甲状腺微小癌262例临床分析[J].中国普通外科杂志, 2016, 25(11):1557–1562. doi:10.3978/j.issn.1005–6947.2016.11.006.Wang ZJ, Li YL, Peng DF, et al. Thyroid microcarcinoma: a clinical analysis of 262 cases[J]. Chinese Journal of General Surgery, 2016,25(11):1557–1562. doi:10.3978/j.issn.1005–6947.2016.11.006.
[20] 翟宝伟, 高庆军, 赵代伟. 甲状腺微小乳头状癌颈部淋巴结转移的危险因素分析[J]. 中国普通外科杂志, 2016, 25(11):1573–1579.doi:10.3978/j.issn.1005–6947.2016.11.009.Zhai BW, Gao QJ, Zhao DW. Analysis of risk factors for cervical lymph node metastases in papillary thyroid microcarcinoma[J].Chinese Journal of General Surgery, 2016, 25(11):1573–1579.doi:10.3978/j.issn.1005–6947.2016.11.009.
[21] Chang YW, Kim HS, Kim HY, et al. Should central lymph node dissection be considered for all papillary thyroid microcarcinoma?[J]. Asian J Surg, 2016, 39(4):197–201. doi:10.1016/j.asjsur.2015.02.006.
[22] 陈征, 吕晶. 甲状腺微小癌颈淋巴结转移危险因素分析及手术范围的探讨[J]. 中国普通外科杂志, 2016, 25(5):659–664.doi:10.3978/j.issn.1005–6947.2016.05.006.Chen Z, Lu J. Analysis of risk factors for cervical lymph node metastasis and the scope of surgical dissection in thyroid microcarcinoma[J]. Chinese Journal of General Surgery, 2016,25(5):659–664. doi:10.3978/j.issn.1005–6947.2016.05.006.
[23] 林晓东, 陈晓意, 黄宝骏, 等. 预防性颈中央区淋巴结清扫对cN0分化型甲状腺癌分期与复发危险度分层的意义[J]. 中国普通外科杂志, 2015, 24(5):633–637. doi:10.3978/j.issn. 1005–6947.2015.05.003.Lin XD, Chen XY, Huang BJ, et al. Significance of prophylactic central lymph node dissection in tumor stage classification and risk stratification of recurrence for cN0 differentiated thyroid carcinoma[J]. Chinese Journal of General Surgery, 2015, 24(5):633–637. doi:10.3978/j.issn.1005–6947.2015.05.003.
