胆囊结石是肝胆外科常见疾病,发病率约为7%[1]。因胆囊结石行胆囊切除的患者中约20%合并胆总管结石(common bile duct stones),其发病率随年龄增长逐渐升高,61~70岁的患者达到31%,71~80岁的患者达到48%[2]。胆囊结石合并胆总管结石的传统术式是胆囊切除、胆总管切开取石、T管引流术,随着腹腔镜技术及内镜技术的快速发展,开腹手术已逐渐被微创术式取代。目前微创术式主要有两种:其一,腹腔镜下胆囊切除术(LC)+胆总管探查取石术(LCBDE);其二,逆行性胰胆管造影(ERCP)/经十二指肠镜Oddi括约肌切开术(EST)+LC[3-4]。当前对两种术式的效果及安全性研究已经有很多且有争议,对于不同年龄段患者的选用标准是否统一尚无共识。本文通过回顾我科近年来收治的老年胆囊结石合并胆总管结石患者的临床资料,对比两种术式,探讨老年胆囊结石合并胆总管结石微创治疗术式的选择。
1 资料与方法
1.1 一般资料
回顾性分析本院肝胆胰外科2012年10月—2 0 1 6年4月诊治的6 0岁以上[5-6]的胆囊结石合并胆总管结石老年患者9 4例,其中4 5例行LC+LCBDE(LC+LCBDE组),49例行ERCP/EST+LC(ERCP/EST+LC组)。LC+LCBDE组男23例,女22例;平均年龄(68.36±5.16)岁。ERCP/EST+LC组男28例,女21例;平均年龄(68.8±5.83)岁。
纳入标准:术前B超、上腹部CT或磁共振胆胰管造影(MRCP)等影像学检查明确诊断为胆囊结石合并胆总管结石。排除标准:⑴ 肝内胆管结石;⑵ 术中探查发现胆管囊状扩张或胆管狭窄;⑶ 合并严重的心、肺、肾等功能障碍,不能耐受手术者;⑷ 有上腹部手术史。
两组患者性别、年龄、最大结石直径、胆管直径、术前总胆红素、丙氨酸转氨酶、术前合并症(腹痛、黄疸、胆源性胰腺炎、胆管炎、高血压、糖尿病、心血管系统疾病)等差异无统计学意义(均P>0.05)(表1)。
表1 两组患者一般资料
Table 1 General data of the two groups of patients
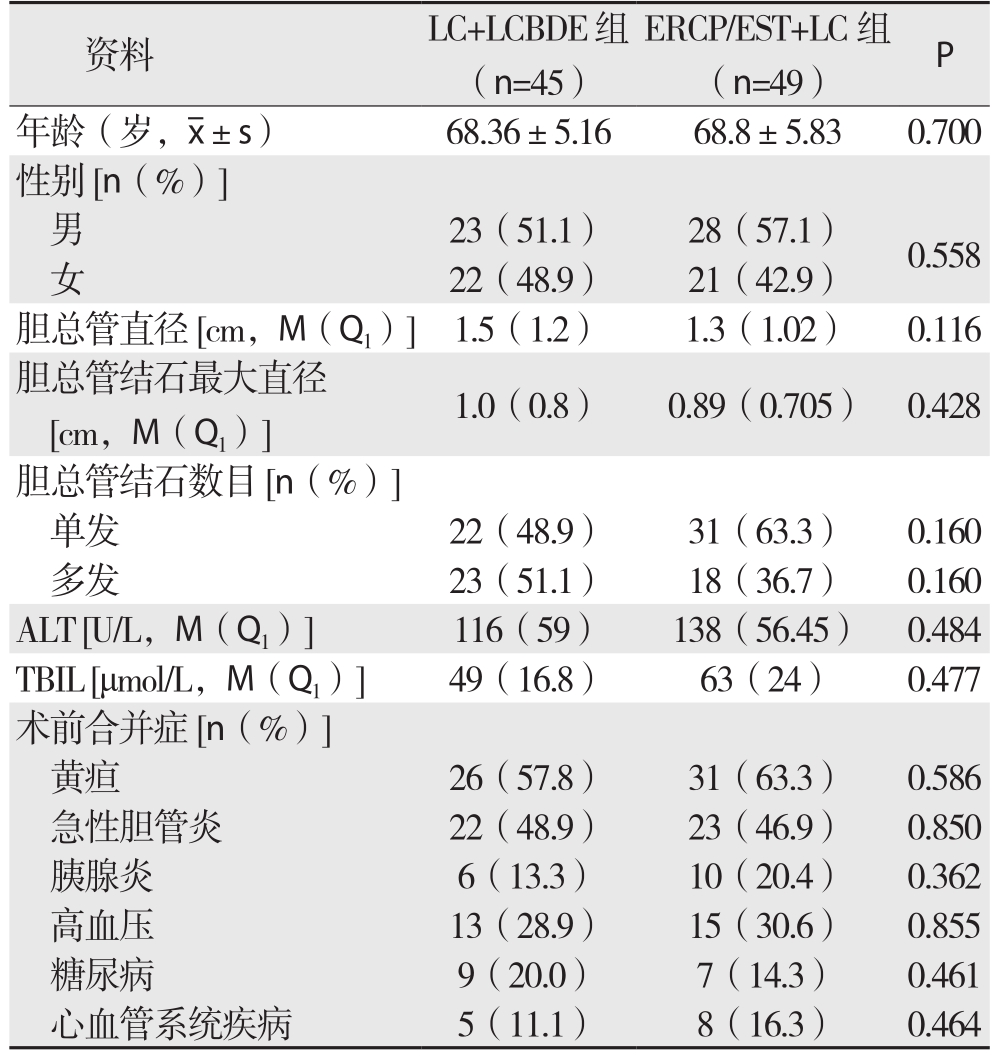
资料 LC+LCBDE组(n=45)ERCP/EST+LC组(n=49) P年龄(岁,x±s) 68.36±5.16 68.8±5.83 0.700性别[n(%)]男23(51.1) 28(57.1) 0.558女22(48.9) 21(42.9)胆总管直径[cm,M(Q1)] 1.5(1.2) 1.3(1.02) 0.116胆总管结石最大直径[cm,M(Q1)] 1.0(0.8) 0.89(0.705) 0.428胆总管结石数目[n(%)]单发 22(48.9) 31(63.3) 0.160多发 23(51.1) 18(36.7) 0.160 ALT [U/L,M(Q1)] 116(59) 138(56.45) 0.484 TBIL [μmol/L,M(Q1)] 49(16.8) 63(24) 0.477术前合并症[n(%)]黄疸 26(57.8) 31(63.3) 0.586急性胆管炎 22(48.9) 23(46.9) 0.850胰腺炎 6(13.3) 10(20.4) 0.362高血压 13(28.9) 15(30.6) 0.855糖尿病 9(20.0) 7(14.3) 0.461心血管系统疾病 5(11.1) 8(16.3) 0.464
1.2 手术方法
1.2.1 LC+LCBDE组 手术采用四孔法,术中维持腹压在12 mmHg(1 mmHg=0.133 kPa),解剖胆囊三角,确切寻及胆囊管及胆囊动脉后,结扎离断胆囊动脉,距离胆总管0.5cm处双重结扎锁夹闭胆囊管,暂不切断胆囊管以做牵引,显露并穿刺明确为胆总管,在十二指肠上缘切开胆总管前壁正中约0.8~1.5cm,术中联合使用纤维胆道镜取石,如结石较大或有嵌顿,可在液电碎石后用网篮取出,最后探查肝内外胆管无结石残留后退出胆道镜,视术中胆道及取石情况一期缝合或留置T管,切断胆囊管,取出胆囊,常规放置肝下缘引流管1根,术后2~3 d拔除,留置T管患者,术后6~8周经T管行胆道照影,确认无残留结石后拔除。
1.2.2 ERCP/EST+LC组 行ERCP,明确胆管解剖情况、结石数目、大小及位置后,在导丝引导下行EST,置入网篮取石,根据结石情况酌情使用碎石取石器或球囊进行取石,再造影未发现残留结石后,留置鼻胆引流管(于LC术后1~2 d造影无异常拔除)。术后常规禁食水24 h,静点抑酸药、生长抑素、抗生素预防急性胰腺炎及胆管炎。监测血、尿淀粉酶变化,血淀粉酶超过正常上限值3倍以上,同时合并典型的胰性腹痛诊断急性胰腺炎[7]。术后2~7 d,若患者病情平稳,血淀粉酶正常,无发热、腹痛、腹胀、恶心呕吐等症状,再行腹腔镜下胆囊切除术(LC)。
1.3 观察指标
比较两组患者手术成功率、结石残留率、住院时间、住院费用、术后并发症发生率,以及远期随访结果。
1.4 统计学处理
使用SPSS 21.0 软件进行统计学分析,计数资料采用χ2检验,计量资料满足正态分布者采用t检验,用均数±标准差![]() 描述,不满足正态分布者采用秩和检验,用中位数(第一四分位数)[M(Q1)]描述,P<0.05为差异有统计学意义。
描述,不满足正态分布者采用秩和检验,用中位数(第一四分位数)[M(Q1)]描述,P<0.05为差异有统计学意义。
2 结 果
2.1 住院治疗情况比较
LC+LCBDE组45例,手术成功42例(包括1例阴性探查,疑为结石术前排入肠道;1例因结石较多无法一次取净而残留结石,于术后6周经T管窦道取石成功),成功率93.3%。胆总管一期缝合3例,留置T管39例。3例中转开腹手术,其中2例炎症较重、腹腔内粘连致密,1例术中出血腹腔镜下无法确切止血。术后出现早期并发症共4例(8.9%),1例因意外牵拉导致T管滑脱,出现胆汁漏,经十二指肠镜置入鼻胆引流管,并充分腹腔引流2周后痊愈。另有胆瘘、切口感染、肺部感染患者各1例,对症处理后治愈。
ERCP/EST+LC组49例,手术成功44例(包括结石残留1例,留置鼻胆引流管7 d后行二次ERCP取净结石;阴性探查2例,疑为结石术前排入肠道),成功率89.8%。ERCP失败3例,2例乳头位于十二指肠憩室插管困难,1例结石过大无法取出,均转行LCBDE。中转开腹2例,由于LC术中肝门区严重粘连,腹腔镜下操作困难。术后出现并发症5例(10.2%),其中急性胰腺炎4例,胆管炎1例,对症支持治疗后好转。
两组患者在手术成功率、结石残留率、术后并发症方面差异均无统计学意义(P>0.05);LC+LCBDE组住院时间(P=0.015)及住院费用(P<0.001)明显少于ERCP/EST+LC组(表2)。
表2 两组治疗结果比较
Table 2 Comparison of the treatment results between the two groups
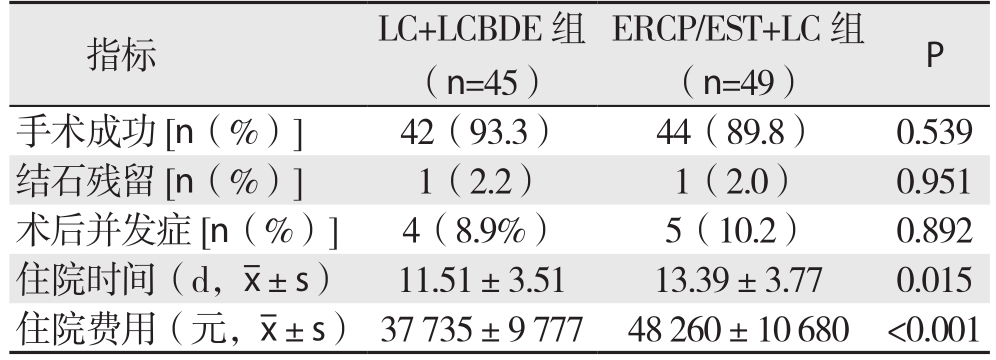
指标 LC+LCBDE组(n=45)ERCP/EST+LC组(n=49) P手术成功[n(%)] 42(93.3) 44(89.8) 0.539结石残留[n(%)] 1(2.2) 1(2.0) 0.951术后并发症[n(%)] 4(8.9%) 5(10.2) 0.892住院时间(d,x±s) 11.51±3.51 13.39±3.77 0.015住院费用(元,x±s) 37 735±9 777 48 260±10 680 <0.001
2.2 远期随访结果
8 1例术后随访6~4 8个月,失访1 3例(LC+LCBDE组6例,ERCP/EST+LC组7例),随访率86.2%。LC+LCBDE组术后1例出现急性胆管炎。ERCP/EST+LC组1例于2年后结石复发,再次行ERCP取石成功,并有1例出现急性胆管炎,另2例死于与本次研究不相关的疾病。两组患者结石复发、胆道感染发生率均无统计学差异(均P>0.05),均未发生胆道狭窄、胰腺炎、胆管恶变(表3)。
表3 两组远期随访结果比较[n(%)]
Table 3 Comparison of the long-term follow-up results between the two groups [n (%)]
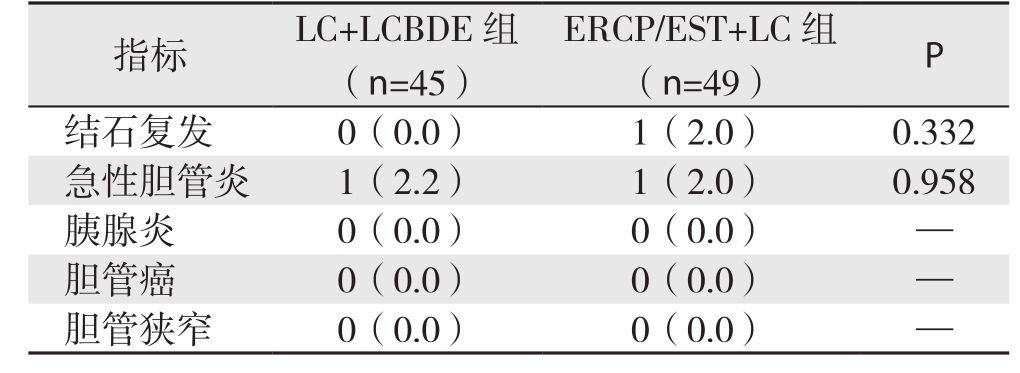
指标 LC+LCBDE组(n=45)ERCP/EST+LC组(n=49) P结石复发 0(0.0) 1(2.0) 0.332急性胆管炎 1(2.2) 1(2.0) 0.958胰腺炎 0(0.0) 0(0.0) —胆管癌 0(0.0) 0(0.0) —胆管狭窄 0(0.0) 0(0.0) —
3 讨 论
LC+LCBDE与ERCP/EST+LC是目前外科治疗胆囊结石合并胆总管结石主要的两种术式,两者同为微创技术,均有创伤小、恢复快、患者痛苦少等优点[8-10]。老年患者病情复杂多变,器官功能衰退,常合并有其他系统疾病,手术风险相对较大,预后差。对于老年患者两种术式哪一种更有优势,值得商榷。
本研究中两组的手术成功率和手术并发症差异不显著,LC+LCBDE组手术成功率93.3%,术后并发症发生率8.9%;ERCP/EST+LC组手术成功率89.8%,术后并发症发生率10.2%,与Bansal等[11]研究的结果相近。LC+LCBDE组平均住院费用(37 735±9 777)元,平均住院时间(11.51±3.51)d(P<0.001);ERCP/EST+LC组平均住院费用(48 260±10 680)元,平均住院时间(13.39±3.77)d(P=0.015)。表明了LC+LCBDE在住院费用及住院时间上的优势。
有研究[12]认为老年患者应用LC+LCBDE与年轻患者同样安全有效。此术式一次手术解决了胆囊和胆管两个问题,创伤小、恢复快。联合使用术中胆道镜可直视胆道内情况,操作方便,成功率高。该术式对结石的数量没有太多限制,且可应用于较大的胆总管结石。本组1例患者最大结石直径达到2.5cm,联合使用术中胆道镜,行液电碎石后取石成功。最大优点是LC+LCBDE不损伤Oddi括约肌,保留了胆道的正常开闭功能。但腹腔镜手术操作复杂,术者需掌握娴熟的操作技术,手术时间长,术后多需要留置T管,由于腹腔镜手术对腹腔脏器的干扰轻,T管形成窦道慢,带管时间较传统开腹手术长,本组患者T管带管时间6~8周,无形中减小了微创的优势,T管胆汁外引流可造成机体生理功能紊乱,且有意外脱落可能,老年患者多有其他系统的疾患,风险较大。本研究中LC+LCBDE组留置T管39例,一期缝合3例,3例一期缝合患者术后恢复良好,均未出现明显并发症。国外有研究[13]发现一期缝合是同样安全有效的,而且一期缝合住院时间和术后并发症发生率都明显降低,国内文献[14]报道一期缝合与放置T 管效果相似,术后住院时间明显缩短,但胆瘘的相关风险因素尚需要大样本的数据资料研究确定,黄强等[15]则认为胆总管结石患者多有过胆道感染病史,一期缝合无法保证胆道低压和无菌。因此临床工作中须严格把握一期缝合的适应证:⑴ 胆总管直径>0.8cm;⑵ 胆总管内无结石残留;⑶ 胆总管下端通畅,无狭窄,胆管壁炎症轻,无明显水肿;⑷ 无胰腺炎、重度黄疸及肝功能损害;⑸ 熟练的腹腔镜下缝合技术[16-17]。
ERCP/EST+LC应用于特定患者有其独到之处,对于合并急性化脓性胆管炎生命体征不稳定或胆源性胰腺炎腹腔内炎症较重的老年患者,腹腔镜胆总管探查术难度大、时间长,手术及麻醉风险较大。而对于此类患者行ERCP留置鼻胆引流管,可迅速解除胆道梗阻,降低黄疸水平,控制胆道感染,待患者临床症状及全身情况好转后,再施行LC。术前行ERCP还可以提前了解胆囊管及胆道情况,为下一步的LC手术提供参考,减少术中损伤胆总管的几率[18]。而且避免了长期带T管,避免了由于胆汁外引流造成的生理功能及水电解质紊乱,减少了胆道逆行感染的可能,提高了术后生活质量。然而EST近期并发症率约为8%~10%[19],包括急性胰腺炎、急性胆管炎、出血、十二指肠穿孔等,其中以急性胰腺炎最为常见。EST切开了Oddi括约肌,破坏了其生理屏障功能,可能导致十二指肠液逆行进入胆总管内,引起多种远期并发症,如胆管炎、胆总管结石复发、胆管癌等[20]。Ding等[21]对221例患者术后随访8~10年认为ERCP/EST+LC组的结石复发率明显高于LC+LCBDE组,Noble等[2]对91例70岁以上的老年患者随访1.38~3.15年发现两组的术后远期并发症无显著差异。而本研究术后随访6~48个月,ERCP/EST+LC组仅1例出现结石复发,两组各出现1例急性胆管炎,无统计学意义。因此两种术式术后远期并发症发生率的差异还须要更多的临床研究来证实。EST有一定的适应证,对于直径<1.5cm,数量少于5枚的胆总管结石,取石成功率高,当结石直径>1.5cm时,耗时长且难度大[22]。LC与ERCP/EST的间隔时间仍然存在着争议,文献[23]报道ERCP/EST取石术后应尽早行LC,胆囊小结石有再次掉入胆总管的风险,且术后3~7 d胆囊及胆囊三角水肿明显,手术难度增加。但笔者认为有效的胆管减压,可减轻胆管炎症,从而减轻腹腔粘连,而且胆囊结石再进入胆总管的几率低,身体一般状态较差的老年患者不能耐受连续的两次手术,因此应根据具体情况确定两次手术的间隔时间。
近年来,相继有LC术中行ERCP/EST的报道,此术式一次手术同时解决胆囊结石和胆总管结石,能缩短住院时间,降低住院费用,更能减少患者的痛苦,避免了等待LC过程中再次继发胆总管结石的可能,若术中ERCP/EST失败,可以立即转行LCBDE或开腹手术[24]。但是术中行ERCP/EST,需具备术中X射线及内镜设备的一体化手术间,内镜医生及外科医生须娴熟配合,同时要在术中调整患者的体位,导致该手术过程较复杂,技术要求更高,目前只有具备相当规模的医院才可能开展,很难推广普及[25]。
LC+LCBDE和ERCP/EST+LC均是治疗胆囊结石合并胆总管结石安全、有效的治疗方案,两者手术成功率、并发症发生率无明显差异。对于多数患者LC+LCBDE住院时间更短,住院费用更低,对胆总管结石的大小、数量无限制,且保护了Oddi括约肌,应作为首选。但对于病情严重合并凝血功能障碍、重度黄疸、急性化脓性胆管炎、胆源性胰腺炎以及心肺功能差的老年患者,ERCP/EST+LC是更好的选择[26]。临床医生应根据老年患者的病情及技术条件灵活选择治疗方案。
参考文献
[1]吕少诚,黄志强.浅谈我国胆道外科的发展现状与展望[J].国际外科学杂志,2014,41(5):289–292.doi:10.3760/cma.j.issn.1673–4203.2014.05.001.Lu SC,Huang ZQ.Brief discussion of development status and future directions of biliary surgery in China[J].International Journal of Surgery,2014,41(5):289–292.doi:10.3760/cma.j.issn.1673–4203.2014.05.001.
[2]Noble H,Tranter S,Chesworth T,et al.A randomized,clinical trial to compare endoscopic sphincterotomy and subsequent laparoscopic cholecystectomy with primary laparoscopic bile duct exploration during cholecystectomy in higher risk patients with choledocholithiasis[J].J Laparoendosc Adv Surg Tech A,2009,19(6):713–720.doi: 10.1089/lap.2008.0428.
[3]王行雁,徐智,王立新,等.胆囊结石合并胆总管结石的外科微创治疗[J].中国微创外科杂志,2012,12(6):515–517.doi:10.3969/j.issn.1009–6604.2012.06.012.Wang XY,Xu Z,Wang LX,et al.Minimal invasive therapy for patients with choledocholithiasis and gallbladder stone[J].Chinese Journal of Minimally Invasive Surgery,2012,12(6):515–517.doi:10.3969/j.issn.1009–6604.2012.06.012.
[4]李宇,郝杰,孙昊,等.一期腹腔镜胆囊切除联合胆总管探查取石与分期内镜取石和腹腔镜胆囊切除术治疗胆囊结石合并胆总管结石的比较[J].中国普通外科杂志,2016,25(2):202–208.doi:10.3978/j.issn.1005–6947.2016.02.008.Li Y,Hao J,Sun H,et al.One-staged laparoscopic cholecystectomy and common bile duct exploration versus two-staged endoscopic stone extraction followed by laparoscopic cholecystectomy for concomitant cholecystolithiasis and choledocholithiasis[J].Chinese Journal of General Surgery,2016,25(2):202–208.doi:10.3978/j.issn.1005–6947.2016.02.008.
[5]杨德盈.老年腹腔镜胆囊切除胆总管探查取石术的临床疗效分析[J].中国普通外科杂志,2015,24(8):1093–1096.doi:10.3978/j.issn.1005–6947.2015.08.007.Yang DY.Clinical efficacy of laparoscopic cholecystectomy and common bile duct exploration for elderly patients with gallbladder disease and concomitant choledocholithiasis[J].Chinese Journal of General Surgery,2015,24(8):1093–1096.doi:10.3978/j.issn.1005–6947.2015.08.007.
[6]黄三雄,吴育连,唐成武,等.两种不同微创方法治疗老年胆囊结石合并胆总管结石的疗效对比[J].中国老年学杂志,2014,34(24):6930–6932.doi:10.3969/j.issn.1005–9202.2014.24.038.Huang SX,Wu LY,Tang CW,et al.Efficacy comparison of two minimally invasive approachs for cholecystolithiasis with choledocholithiasis in elderly patients[J].Chinese Journal of Gerontology,2014,34(24):6930–6932.doi:10.3969/j.issn.1005–9202.2014.24.038.
[7]中华医学会外科学分会胰腺外科学组.急性胰腺炎诊治指南(2014)[J].中国实用外科杂志,2015,35(1):4–7.Pancreatic Surgery Group of Surgery Branch of Chinese Medical Association.Guidelines for diagnosis and treatment of acute pancreatitis (2014)[J].Chinese Journal of Practical Surgery,2015,35(1):4–7.
[8]刘清波,王卫东,陈小伍,等.胆总管结石合并胆囊结石的两种不同处理方法的对比[J].岭南现代临床外科,2014,14(3):267–270.doi:10.3969/j.issn.1009–976X.2014.03.011.Liu QB,Wang WD,Chen XW,et al.Comparison of two different methods for the management of cholecysto-choledocholithiasis[J].Lingnan Modern Clinics in Surgery,2014,14(3):267–270.doi:10.3969/j.issn.1009–976X.2014.03.011.
[9]赵云,杨成林,冯以斌,等.十二指肠镜联合腹腔镜治疗老年胆囊结石合并肝外胆管结石[J].中国普通外科杂志,2016,25(8):1105–1111.doi:10.3978/j.issn.1005–6947.2016.08.003.Zhao Y,Yang CL,Feng YB,et al.Therapeutic combined use of duodenoscopy and laparoscopy for elderly patients with gallbladder stones and concomitant extrahepatic bile duct stones[J].Chinese Journal of General Surgery,2016,25(8):1105–1111.doi:10.3978/j.issn.1005–6947.2016.08.003.
[10]钟伟,倪谢根.腹腔镜联合纤维胆道镜与开腹手术治疗老年胆总管结石对术后疼痛及胃肠功能的影响[J].中国普通外科杂志,2015,24(2):280–283.doi:10.3978/j.issn.1005–6947.2015.02.024.Zh o n g W,Ni X G.L ap ar o sco p y co m bi ne d w it h fibercholedochoscopy and conventional laparotomy for treatment of common bile duct stones in the elderly: effect on postoperative pain and gastrointestinal function[J].Chinese Journal of General Surgery,2015,24(2):280–283.doi:10.3978/j.issn.1005–6947.2015.02.024.
[11]Bansal VK,Misra MC,Garg P,et al.A prospective randomized trial comparing two-stage versus single-stage management of patients with gallstone disease and common bile duct stones[J].Surg Endosc,2010,24(8):1986–1989.doi: 10.1007/s00464–010–0891–7.[12]Lee A,Min SK,Park JJ,et al.Laparoscopic common bile duct exploration for elderly patients:as a first treatment strategy for common bile duct stone[J].J Korean Surg Soc,2011,81(2):128–133.doi: 10.4174/jkss.2011.81.2.128.
[13]Khaled YS,Malde DJ,de Souza C,et al.Laparoscopic bile duct exploration via choledochotomy followed by primary duct closure is feasible and safe for the treatment of choledocholithiasis[J].Surg Endosc,2013,27(11):4164–4170.doi: 10.1007/s00464–013–3015–3.
[14]潘峥,程张军,刘胜利,等.胆总管结石腹腔镜胆总管探查术后一期缝合与T管引流的临床比较[J].中国普通外科杂志,2015,24(8):1135–1139.doi:10.3978/j.issn.1005–6947.2015.08.016.Pan Z,Cheng ZJ,Liu SL,et al.Primary closure versus T-tube drainage following laparoscopic common bile duct exploration for choledocholithiasis[J].Chinese Journal of General Surgery,2015,24(8):1135–1139.doi:10.3978/j.issn.1005–6947.2015.08.016.
[15]黄强,刘臣海.胆总管结石的微创化治疗[J].肝胆外科杂志,2013,21(2):86–88.doi:10.3969/j.issn.1006–4761.2013.02.003.Huang Q,Liu CH.Minimally invasive therapy for common bile duct stones[J].Journal of Hepatobiliary Surgery,2013,21(2):86–88.doi:10.3969/j.issn.1006–4761.2013.02.003.
[16]王广义,邱伟,吕国悦.胆囊结石合并胆总管结石的微创治疗[J].外科理论与实践,2013,18(2):112–114.Wang GY,Qiu W,Lu GY.Minimally invasive therapy for gallbladder and common bile duct stones[J].Journal of Surgery Concepts & Practice,2013,18(2):112–114.
[17]温军业,张海强,脱红芳,等.腹腔镜胆总管切开取石一期缝合的研究进展[J].中国普通外科杂志,2016,25(8):1213–1218.doi:10.3978/j.issn.1005–6947.2016.08.022.Wen JY,Zhang HQ,Tuo HF,et al.Progress of laparoscopic choledochotomy with primary closure[J].Chinese Journal of General Surgery,2016,25(8):1213–1218.doi:10.3978/j.issn.1005–6947.2016.08.022.
[18]Mann K,Belgaumkar AP,Singh S.Post-endoscopic retrograde cholangiography laparoscopic cholecystectomy:challenging but safe[J].JSLS,2013,17(3):371–375.doi: 10.4293/108680813X1365 4754535511.
[19]王中魁,赵海鹰,刘金钢,等.老年人胆囊结石合并胆总管结石术式选择探讨(附60例报告)[J].中国实用外科杂志,2015,35(4):448–450.Wang ZK,Zhao HY,Liu JG,et al.Comparison of operative methods for older patients with concomitant cholelithiasis and choledocholithiasis: A report of 60 patients[J].Chinese Journal of Practical Surgery,2015,35(4):448–450.
[20]Oh HC,Cheon YK,Cho YD,et al.Use of udenafil is not associated with a reduction in post-ERCP pancreatitis: results of a randomized,placebo-controlled,multicenter trial[J].Gastrointest Endosc,2011,74(3):556–562.doi: 10.1016/j.gie.2011.04.047.
[21]Ding G,Cai W,Qin M.Single-stage vs.two-stage management for concomitant gallstones and common bile duct stones:a prospective randomized trial with long-term follow-up[J].J Gastrointest Surg,2014,18(5):947–951.doi: 10.1007/s11605–014–2467–7.
[22]谢凯祥,涂湘炎,汤俊,等.三镜联合治疗胆囊并胆总管结石的临床研究[J].中国内镜杂志,2008,14( 9):970–973.Xie KX,TU XY,Tang J,et al.Clinical observation of combination of three endoscopes in treatment of cholecystolithiasis with choledocholithiasis[J].China Journal of Endoscopy,2008,14(9):970–973.
[23]黄小龙,韩霖,翁杰,等.ERCP联合LC治疗胆囊结石合并胆总管结石34例临床分析[J].海南医学,2011,22(4):70–72.doi:10.3969/j.issn.1003–6350.2011.04.032.Huang XL,Han L,Weng J,et al.Effect of endoscopic retrograde cholangiopancreatography combined with laparoscopic cholecystectomy in the treatment of common bile duct stone complicated with cholecystolithiasis[J].Hainan Medical Journal,2011,22(4):70–72.doi:10.3969/j.issn.1003–6350.2011.04.032.
[24]许松欣,丁岩冰.腹腔镜联合内镜治疗胆囊结石合并胆总管结石的诊治进展[J].中国微创外科杂志,2015,15(4):376–379.doi:10.3969/j.issn.1009–6604.2015.04.027.Xu SX,Ding YB.Development in laparoscopy combined with endoscopy for cholecystolithiasis with choledocholithiasis[J].Chinese Journal of Minimally Invasive Surgery,2015,15(4):376–379.doi:10.3969/j.issn.1009–6604.2015.04.027.
[25]朱杰高,韩威,张忠涛,等.胆囊结石合并胆总管结石的治疗新进展[J].中国全科医学,2013,16(15):1702–1704.doi:10.3969/j.issn.1007–9572.2013.05.079.Zhu JG,Han W,Zhang ZT,et al.Latest development of treatment for cholecystolithiasis combined with choledocholithiasis[J].Chinese General Practice,2013,16(15):1702–1704.doi:10.3969/j.issn.1007–9572.2013.05.079.
[26]Samardzic J,Latic F,Kraljik D,et al.Treatment of common bile duct stones--is the role of ERCP changed in era of minimally invasive surgery[J].Med Arh,2010,64(3):187–188.